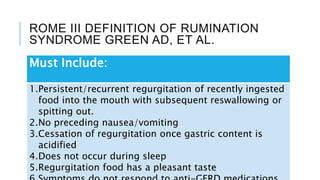
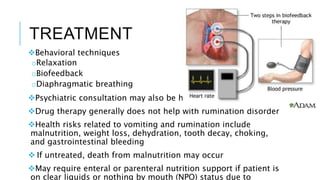
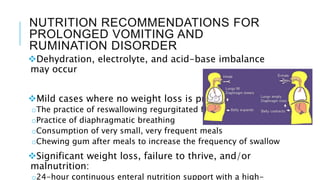
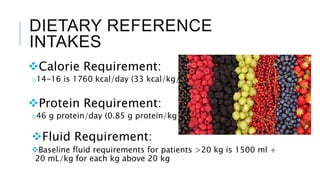
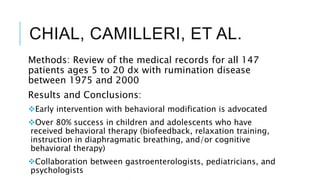
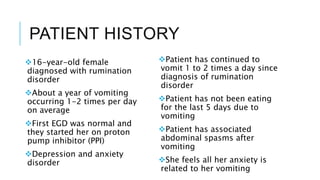
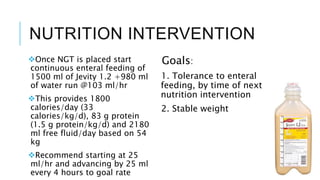
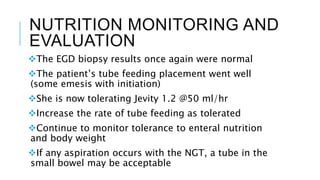
This document discusses rumination disorder in a 16-year-old female patient. Rumination disorder involves repeatedly regurgitating and rechewing or reswallowing food after eating. It is considered a learned behavior rather than a medical condition. Treatment involves behavioral therapy like relaxation techniques and diaphragmatic breathing. For severe cases with weight loss, enteral nutrition may be needed. Multidisciplinary teams including nutrition, psychology, and gastroenterology have been shown to help patients learn to stop the rumination behavior through programs that focus on eating skills.