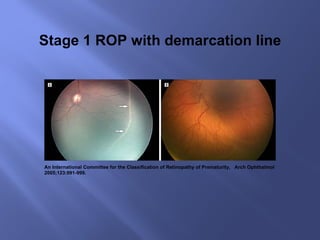
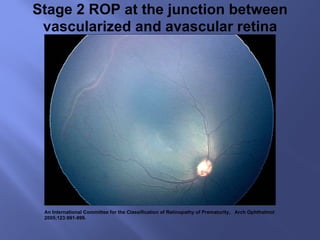
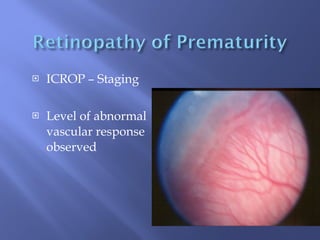
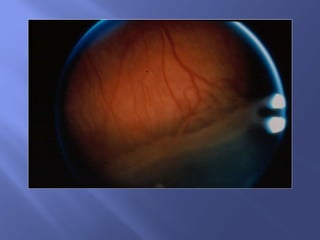
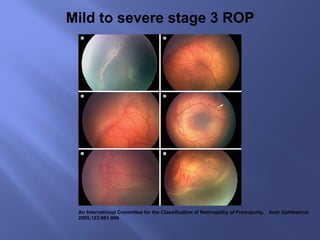
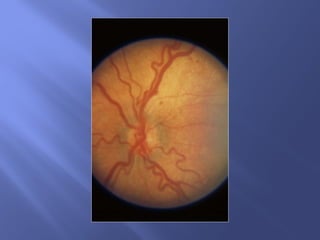
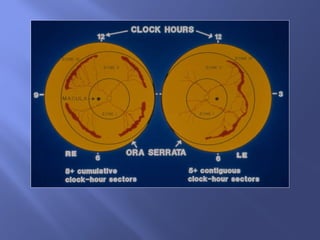
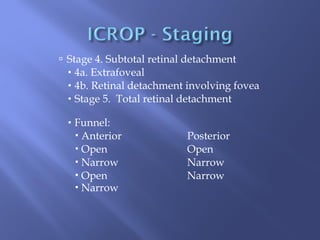
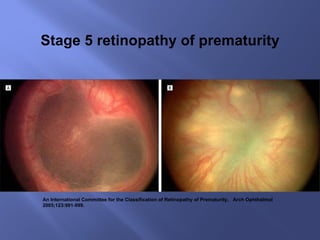
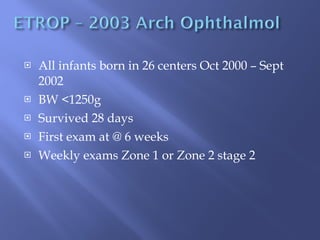
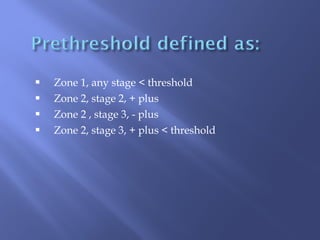
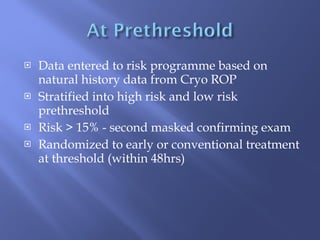
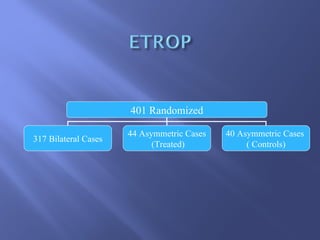
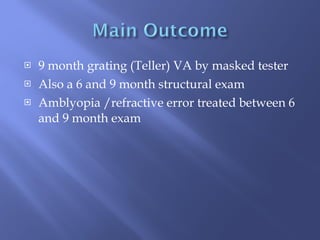
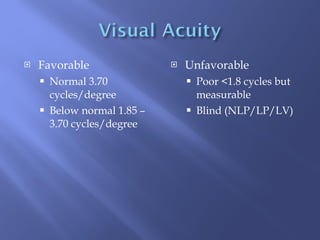
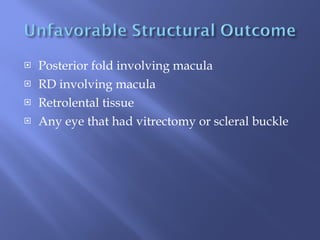
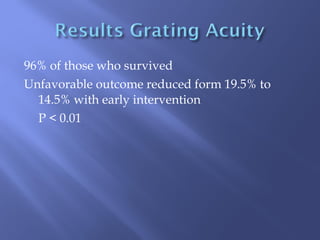
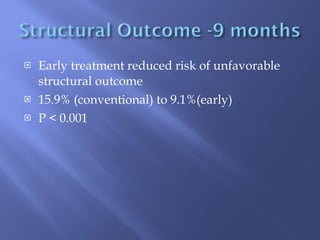
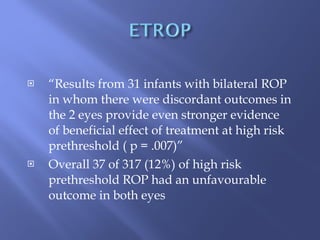
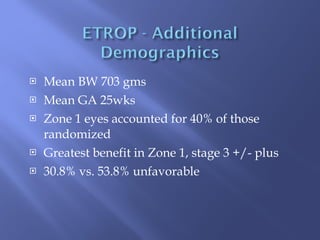
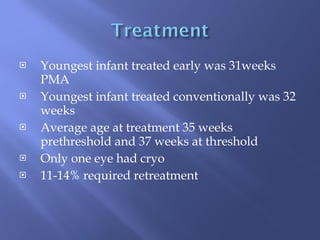
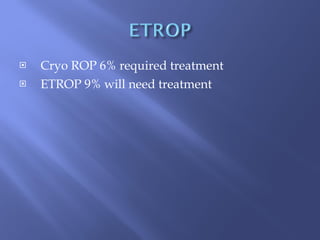
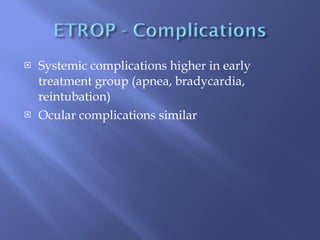
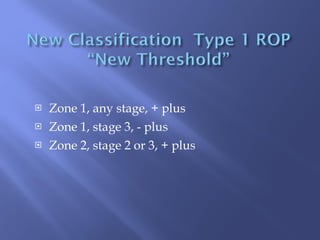
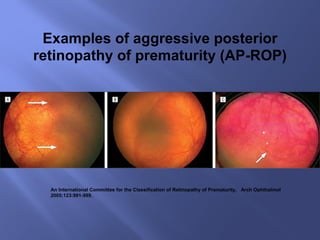
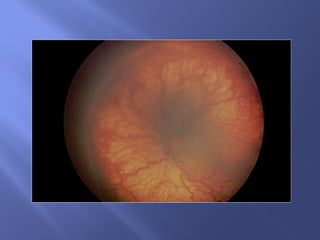
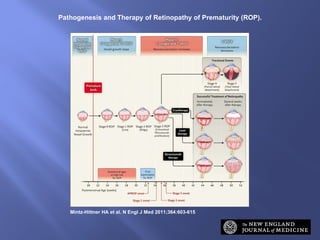
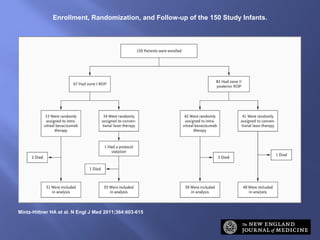
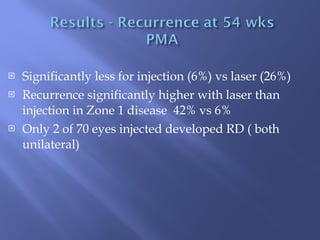
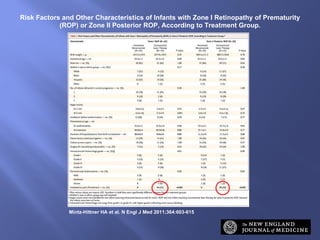
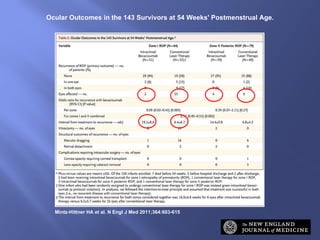
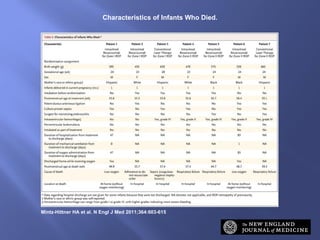
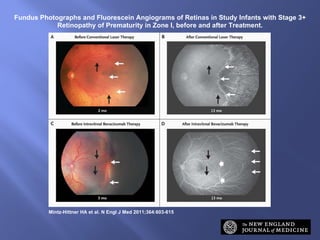
The document discusses the classification and treatment of retinopathy of prematurity (ROP), focusing on various stages and outcomes based on different treatment strategies like early intervention and intravitreal bevacizumab. It highlights the effectiveness of early treatment in reducing unfavorable outcomes and compares the efficacy of bevacizumab with conventional laser therapy. The study concludes that bevacizumab may be more effective for zone I ROP while noting concerns about systemic safety and recurrence risks.