This document summarizes the key issues regarding DNACPR (Do Not Attempt Cardiopulmonary Resuscitation) orders and proposes an alternative approach called the Universal Form of Treatment Options (UFTO). The summary includes:
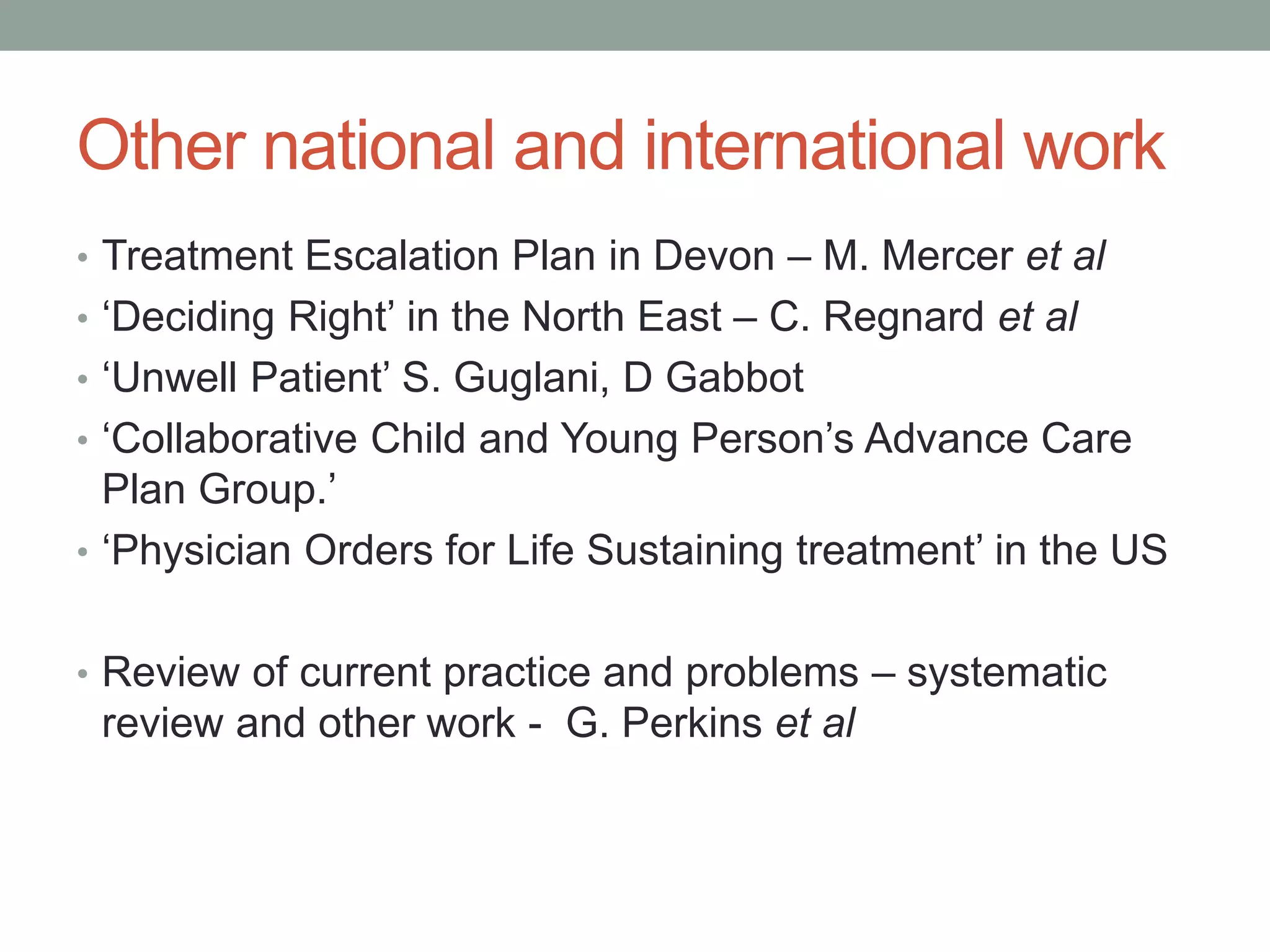
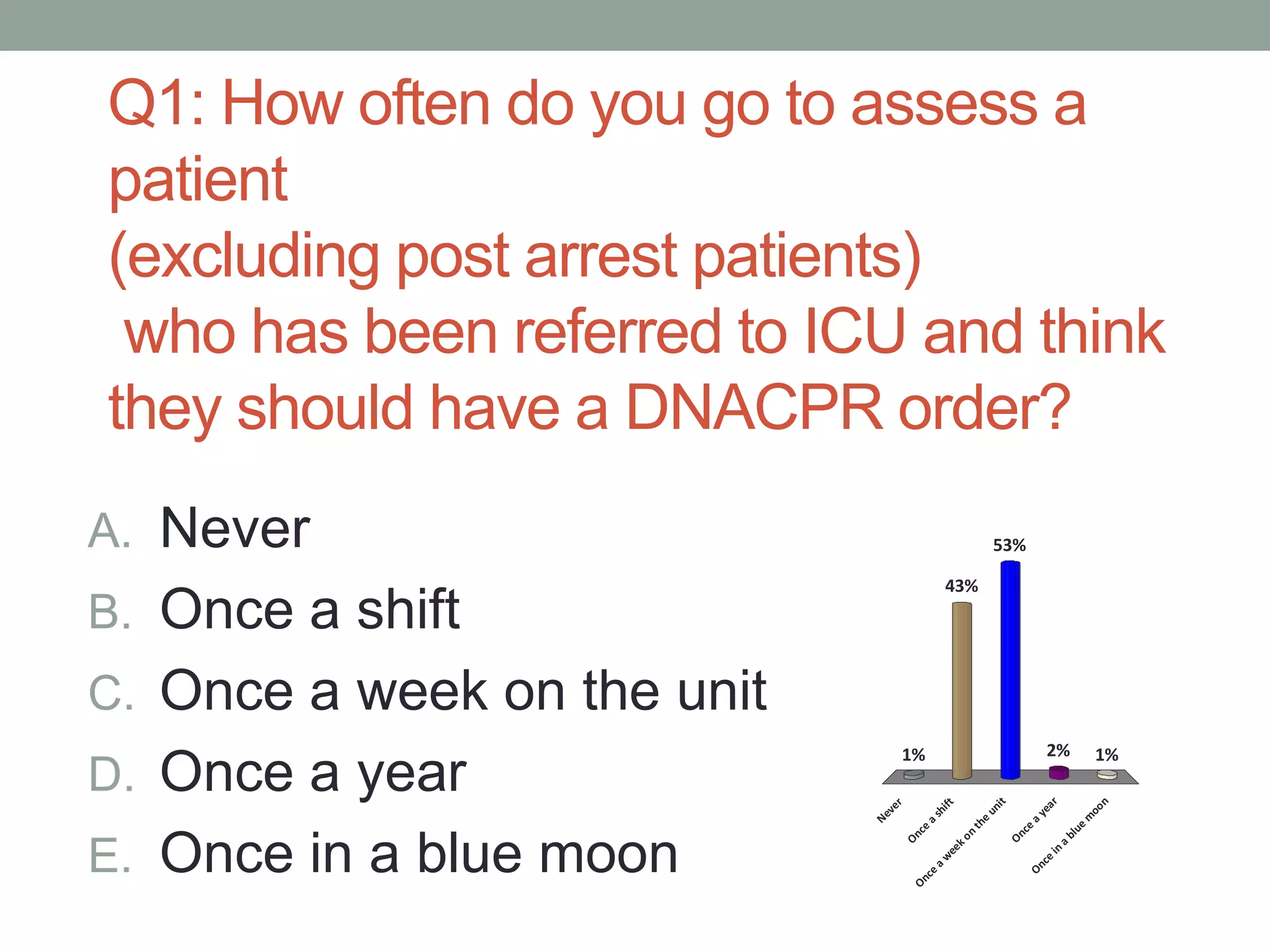
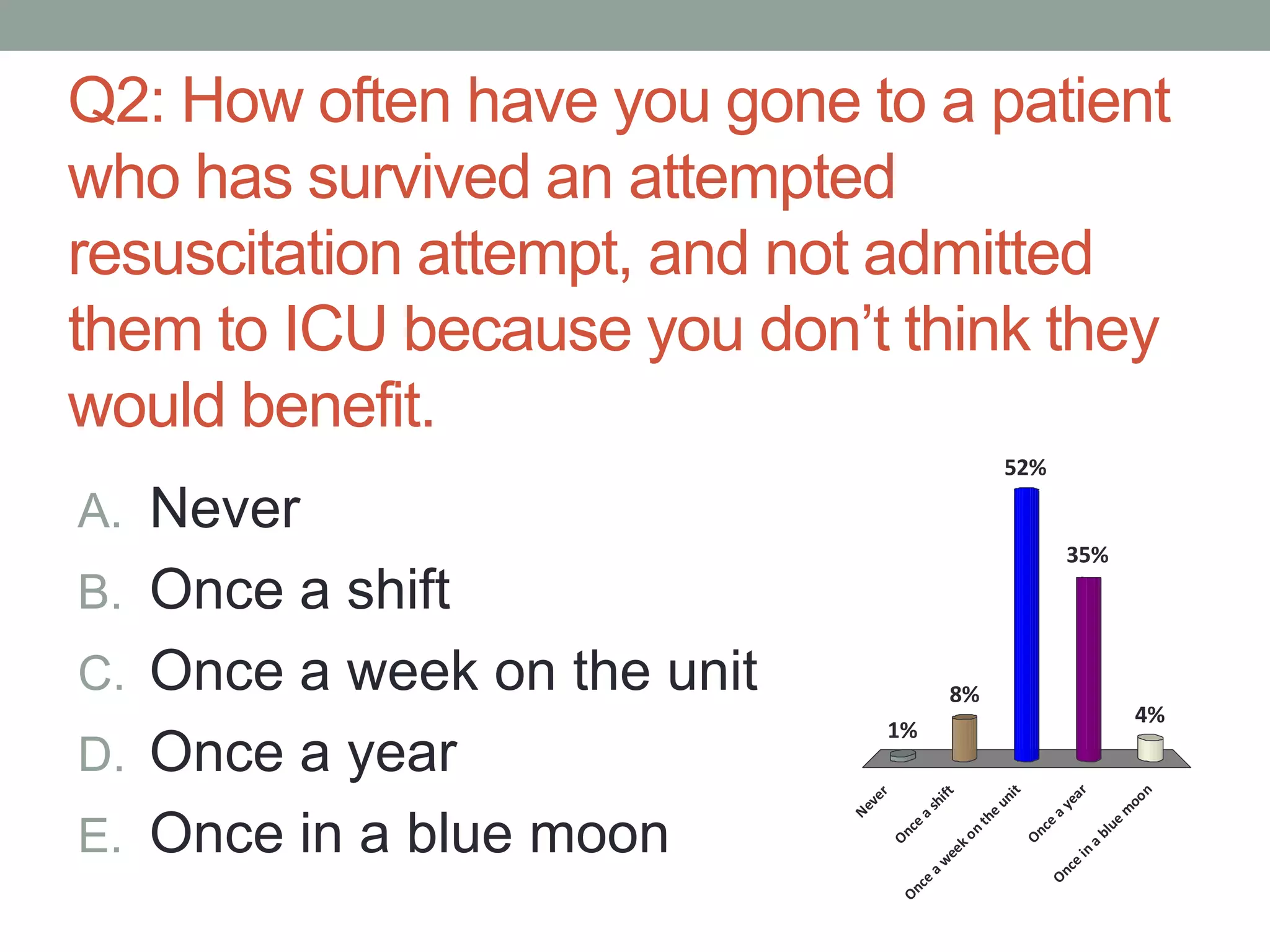
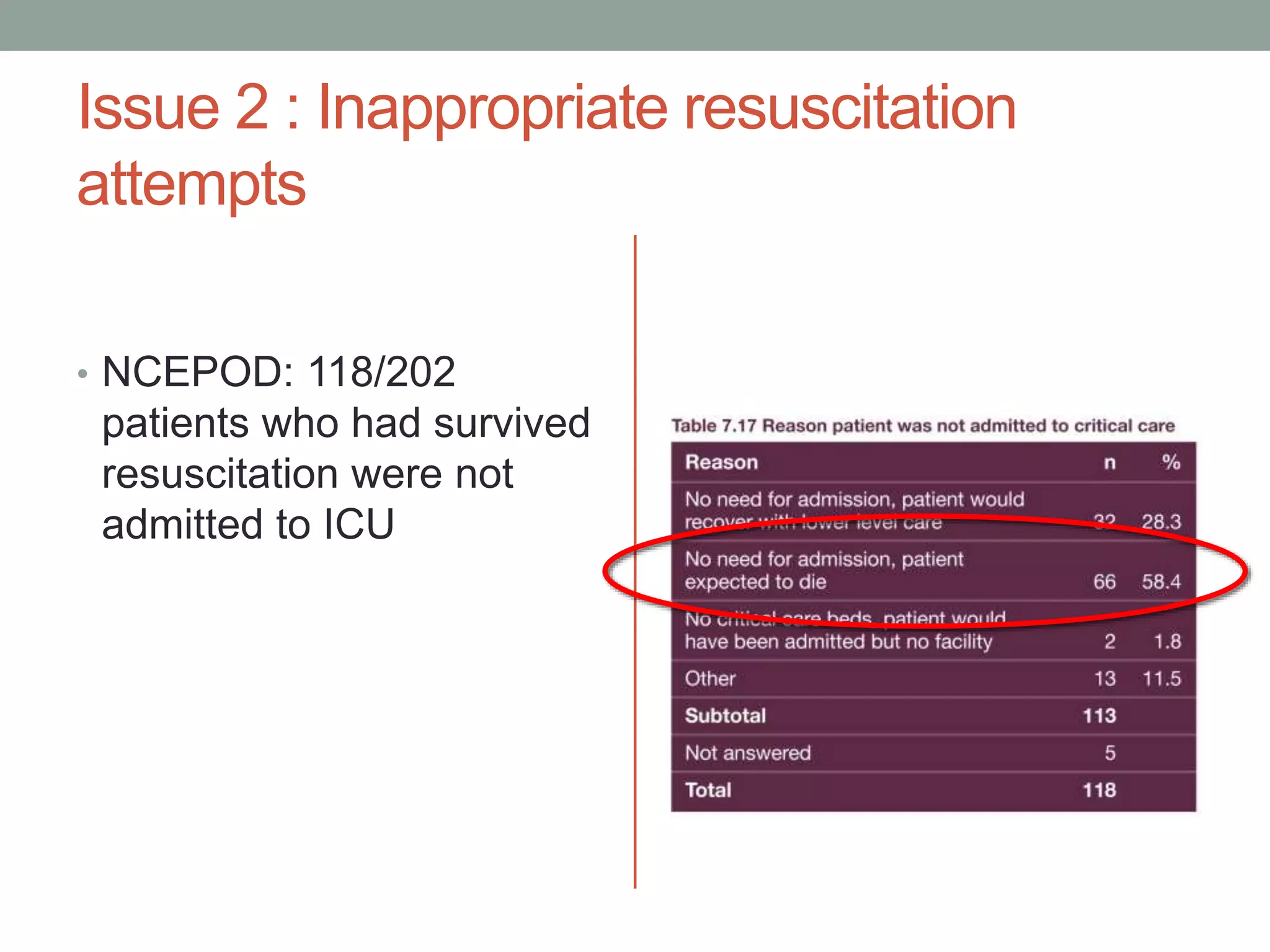
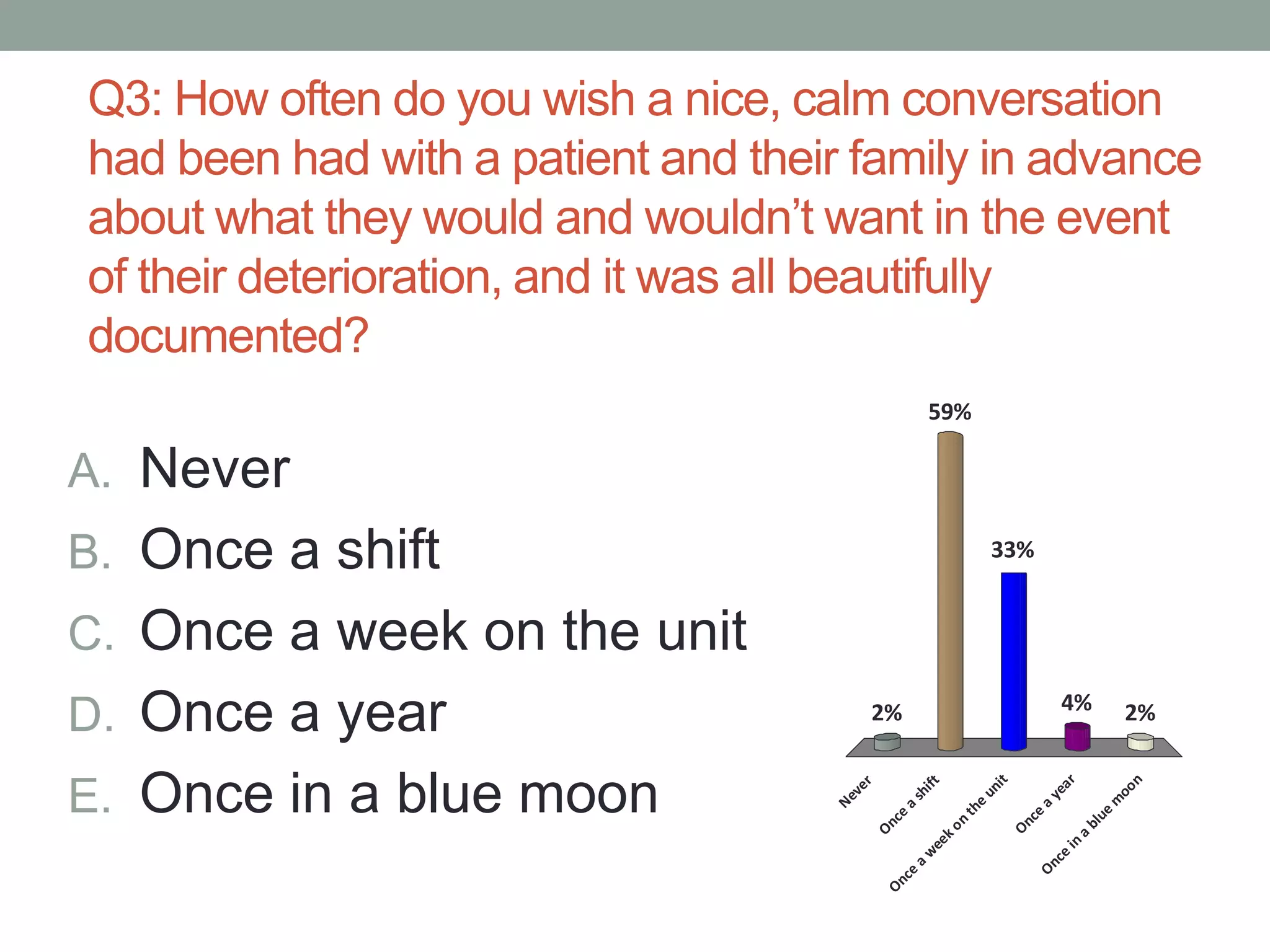
1. There are several ethical issues with the current use of DNACPR orders, including that they are not routinely completed for patients, sometimes result in inappropriate resuscitation attempts, and often lack discussions with patients and families.
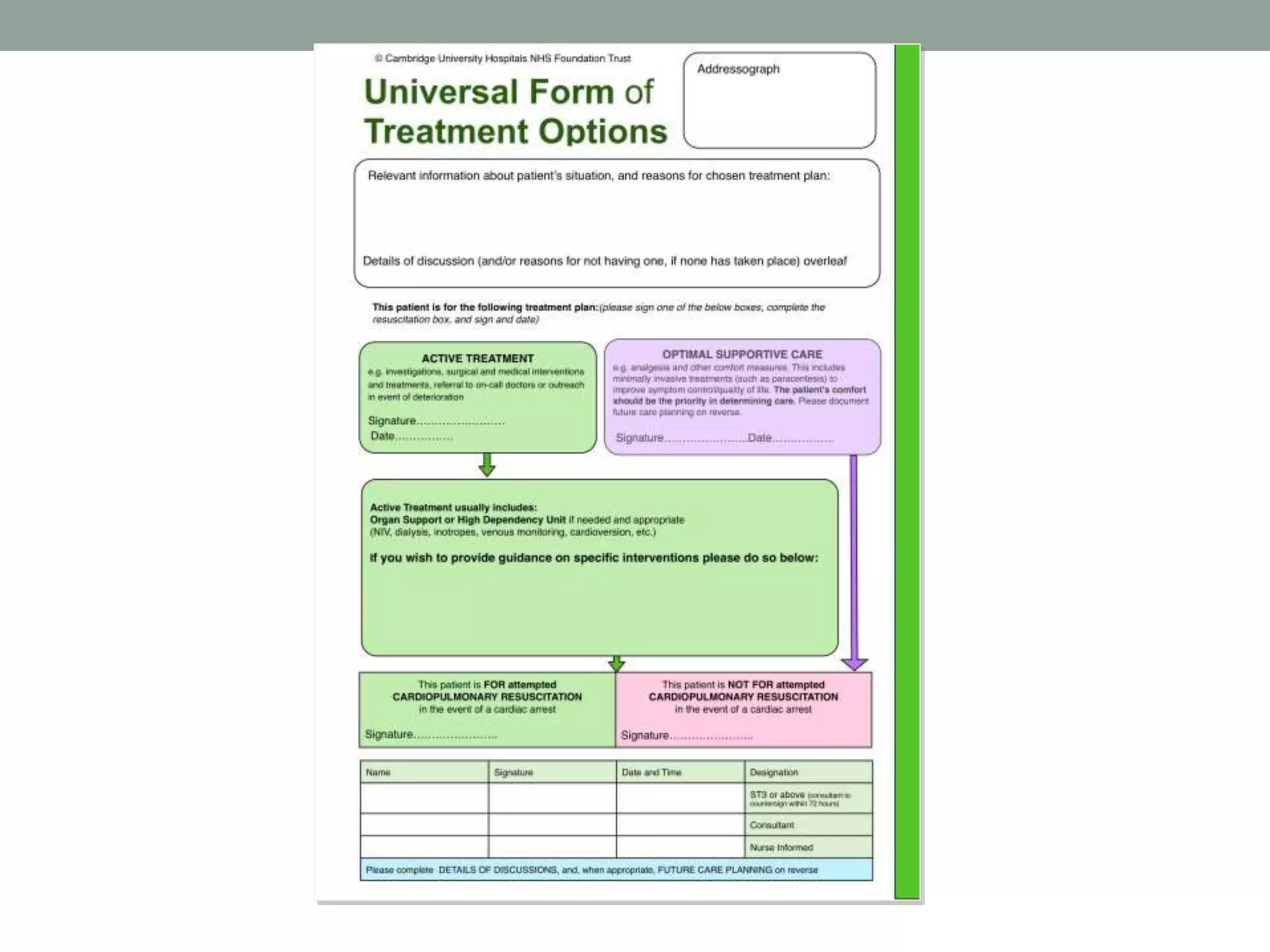
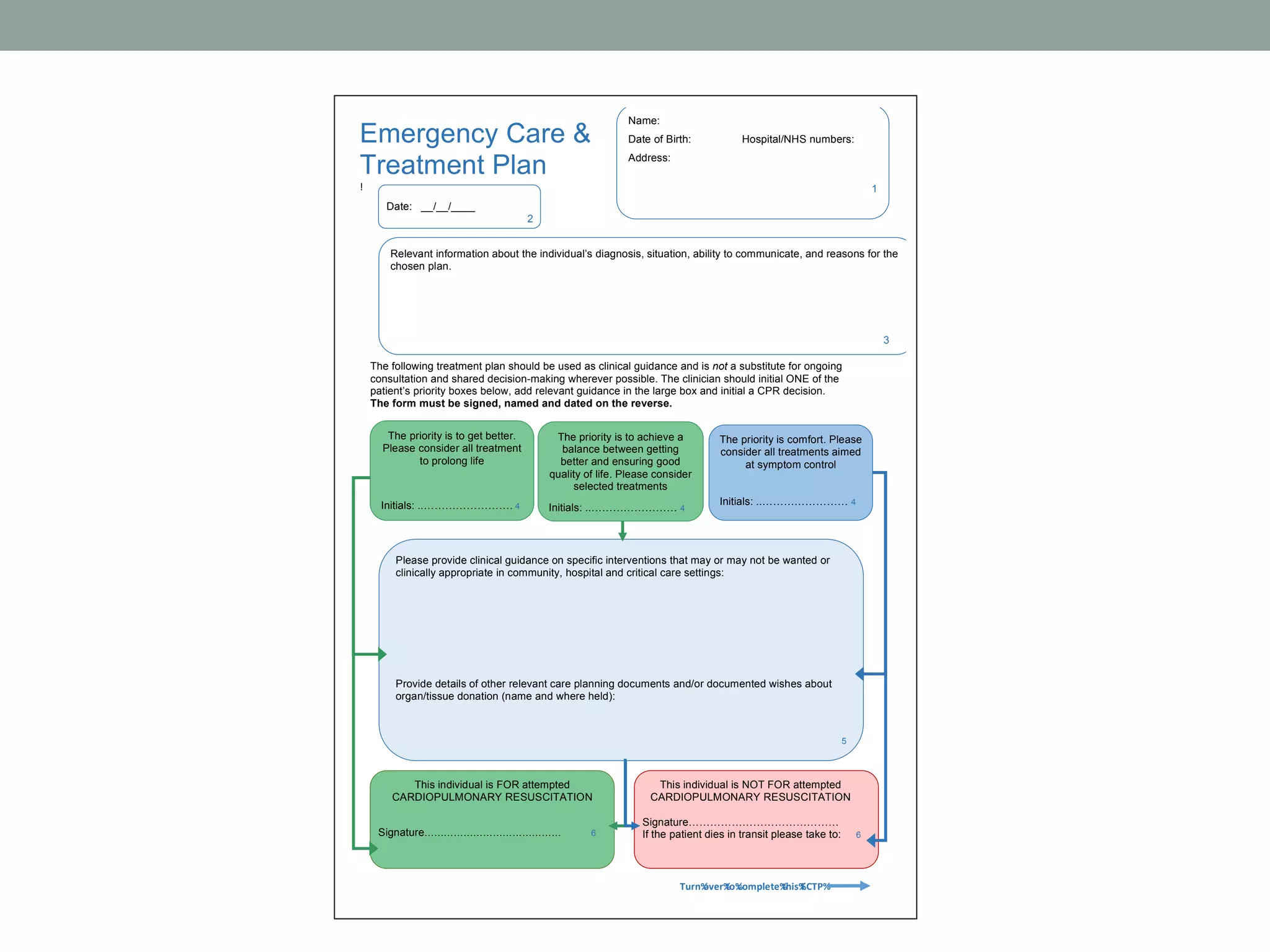
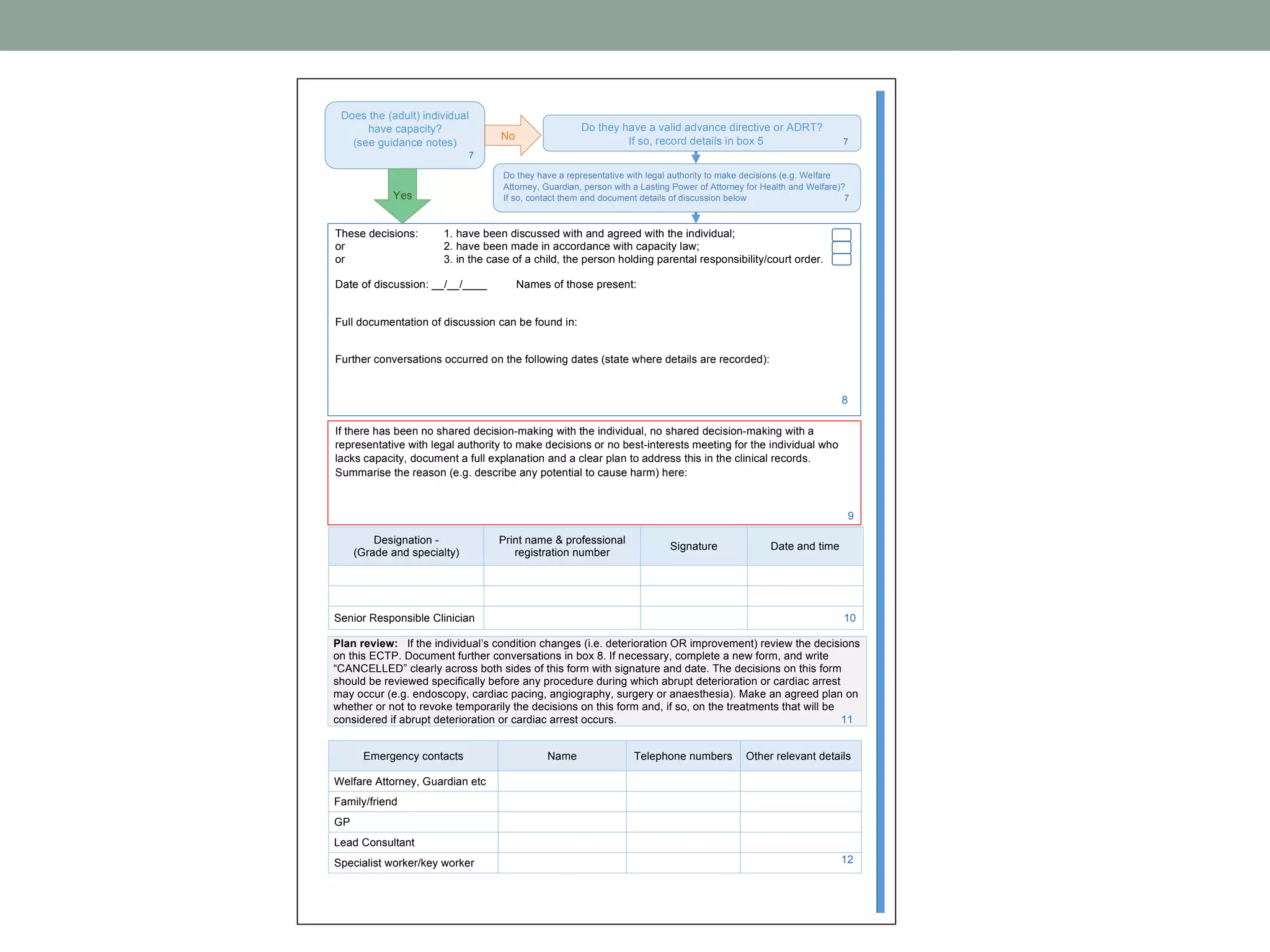
2. The document proposes the UFTO as an alternative, which aims to remove the ad hoc nature of consideration, improve discussions, and shift the focus to goals of care rather than a "resus/no resus" decision.
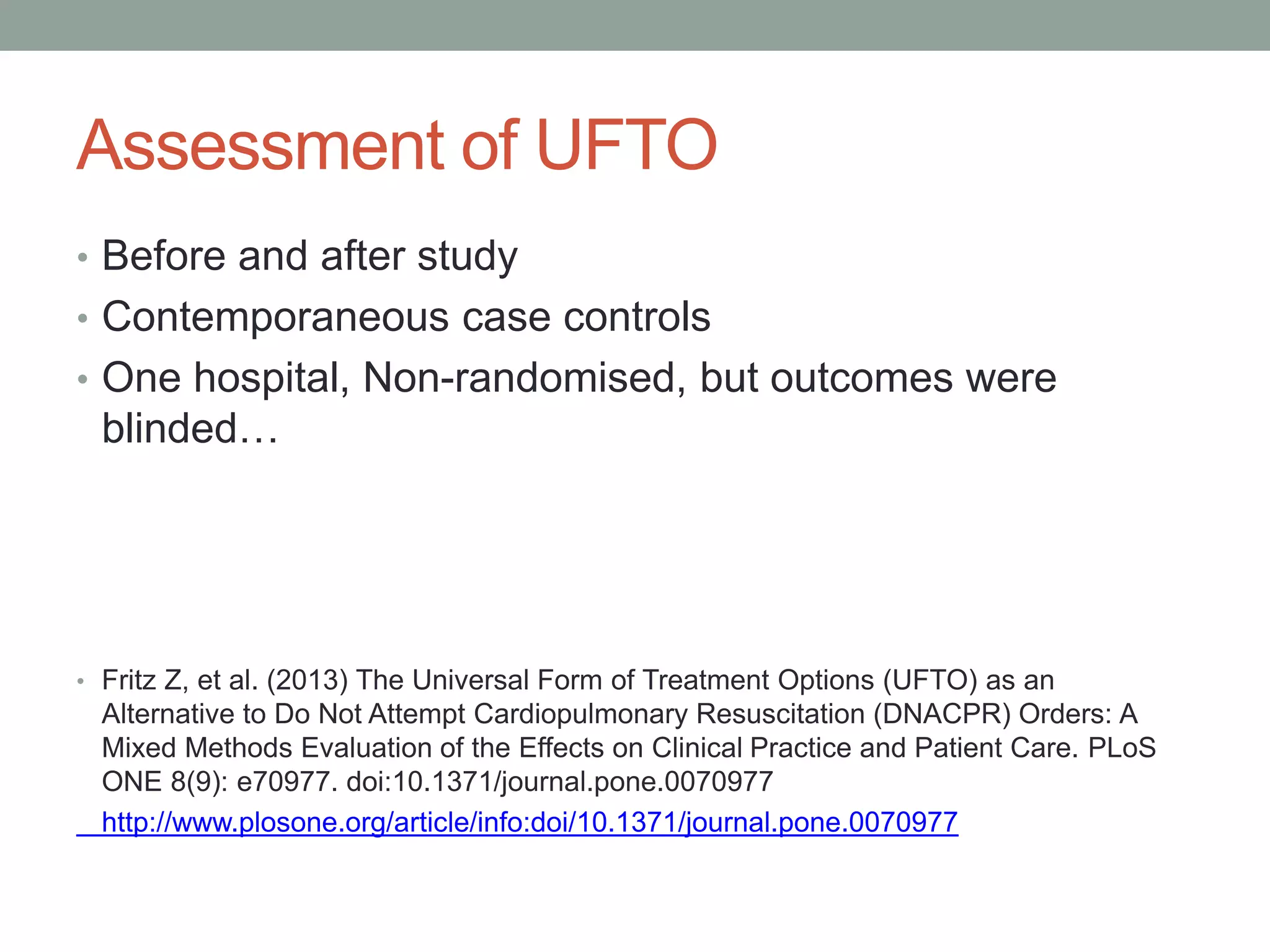
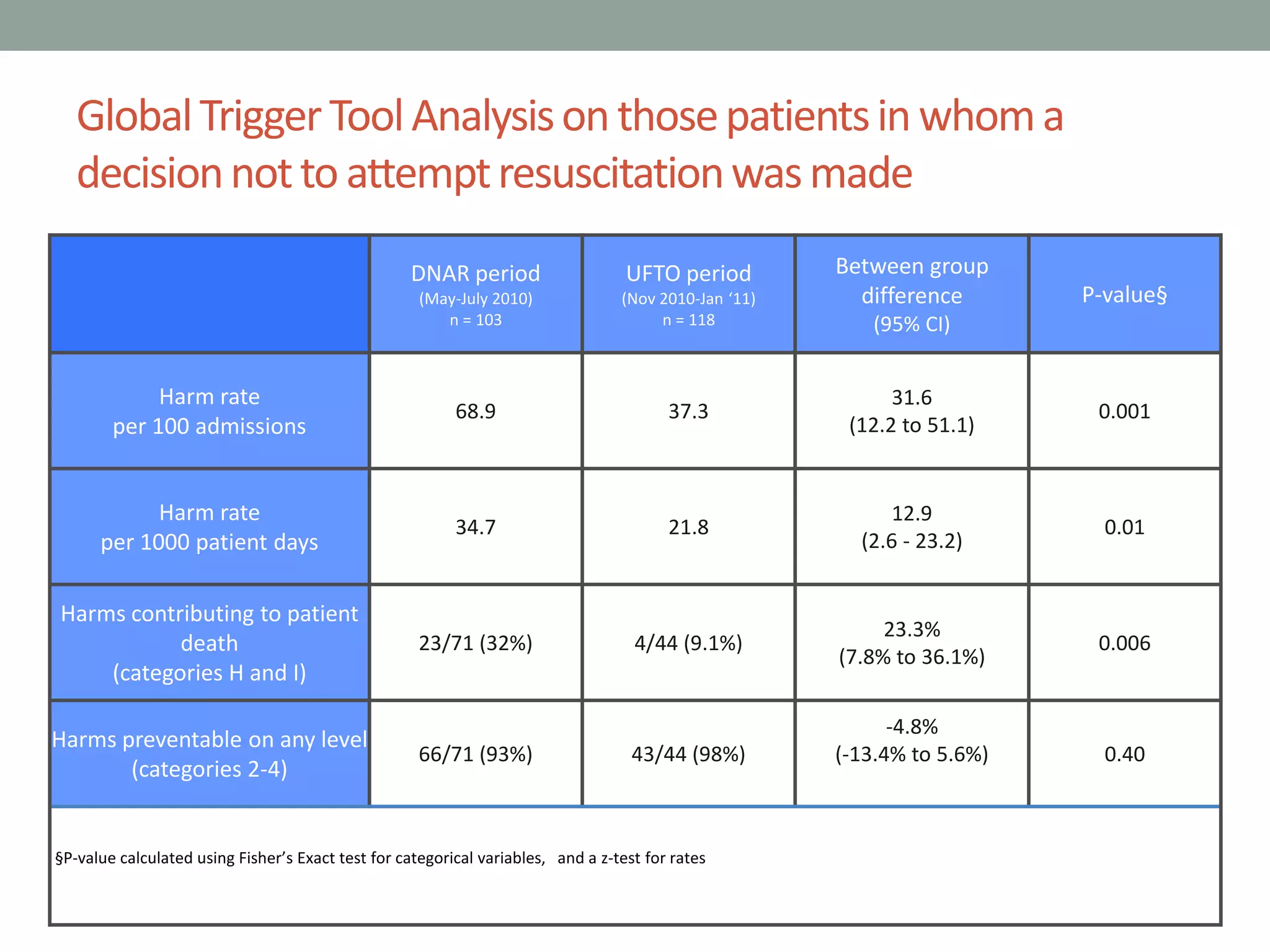
3. A study
![Tracey
• Must discuss unless you think it would cause physiological
or psychological harm – to not do so would be in breach of
article 8 of Human Rights Act
• If you don’t tell a patient that you have made a decision,
you are depriving them of the right to question it, and the
right to ask for a second opinion
• This extends to other treatments as well
• Other areas of non disclosure to be challenged?
• R(Tracey) v Cambridge University Hospital NHS FT and others [2014] EWCA Civ 822 )](https://image.slidesharecdn.com/tue-0945-zoefritz-withvoting-engvoted-151214104507/75/Rethinking-DNACPR-orders-ethical-issues-and-a-proposal-for-change-Fritz-13-2048.jpg)
![Winspear
• If a patient does not have capacity:
• Don’t make a ‘holding decision’ and wait ‘til the morning
• As long as it is ‘practicable and appropriate’ call someone who
knows them
Winspear v City Hospitals Sunderland NHS FT
[2015] EWHC 3250 (QB)](https://image.slidesharecdn.com/tue-0945-zoefritz-withvoting-engvoted-151214104507/75/Rethinking-DNACPR-orders-ethical-issues-and-a-proposal-for-change-Fritz-14-2048.jpg)