This document summarizes a presentation on palliative care and code status discussions. It begins with objectives to introduce palliative care at the hospital and improve comfort discussing code status. It defines palliative care and common misconceptions. Data is presented showing benefits of palliative care like improved quality of life. The document then discusses code status, presenting survival rates for CPR, which are quite low especially for older patients. It provides guidance on having informed code status discussions that address patient goals, expectations and alternatives. Resources for these important conversations are also listed.
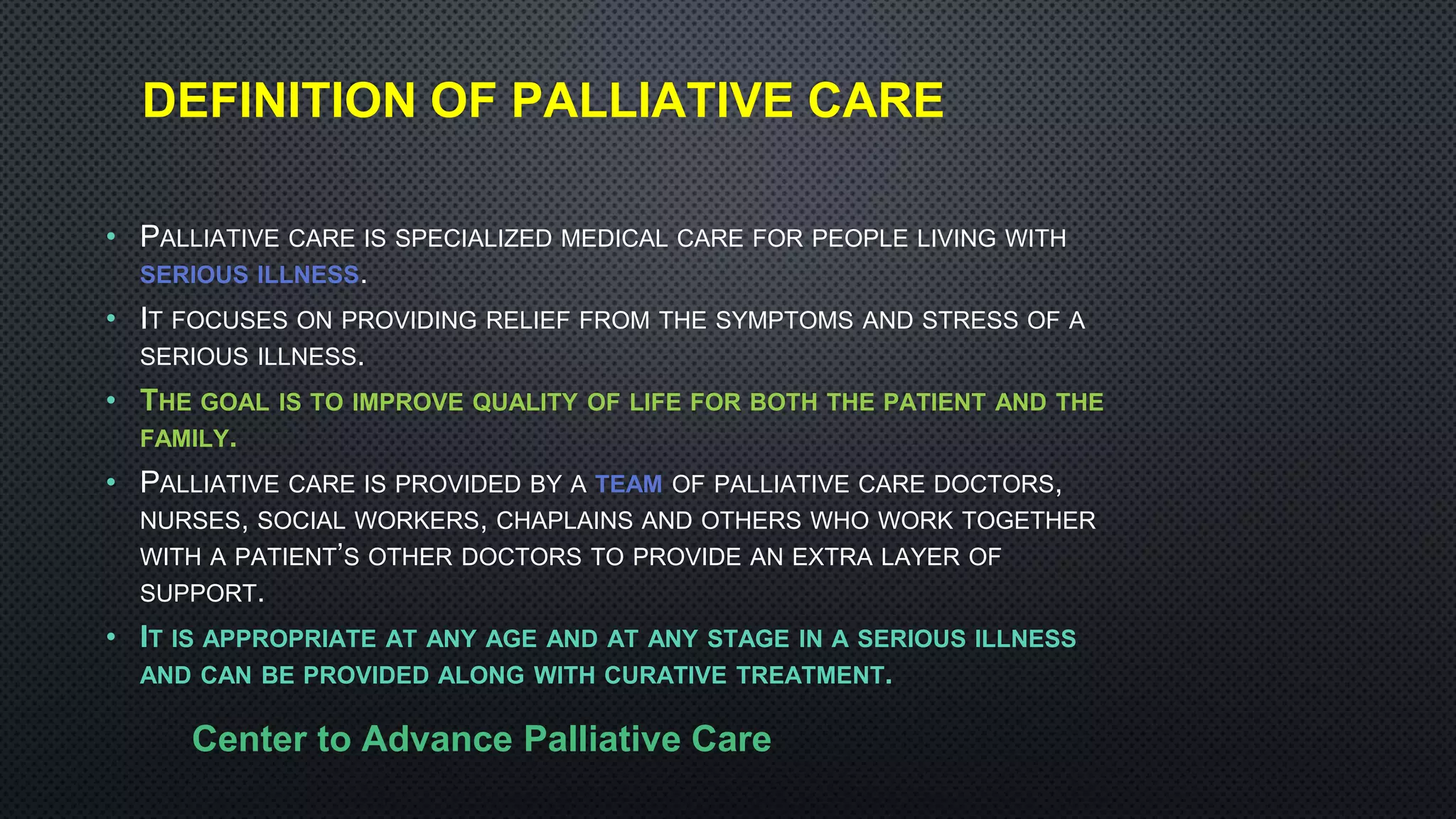


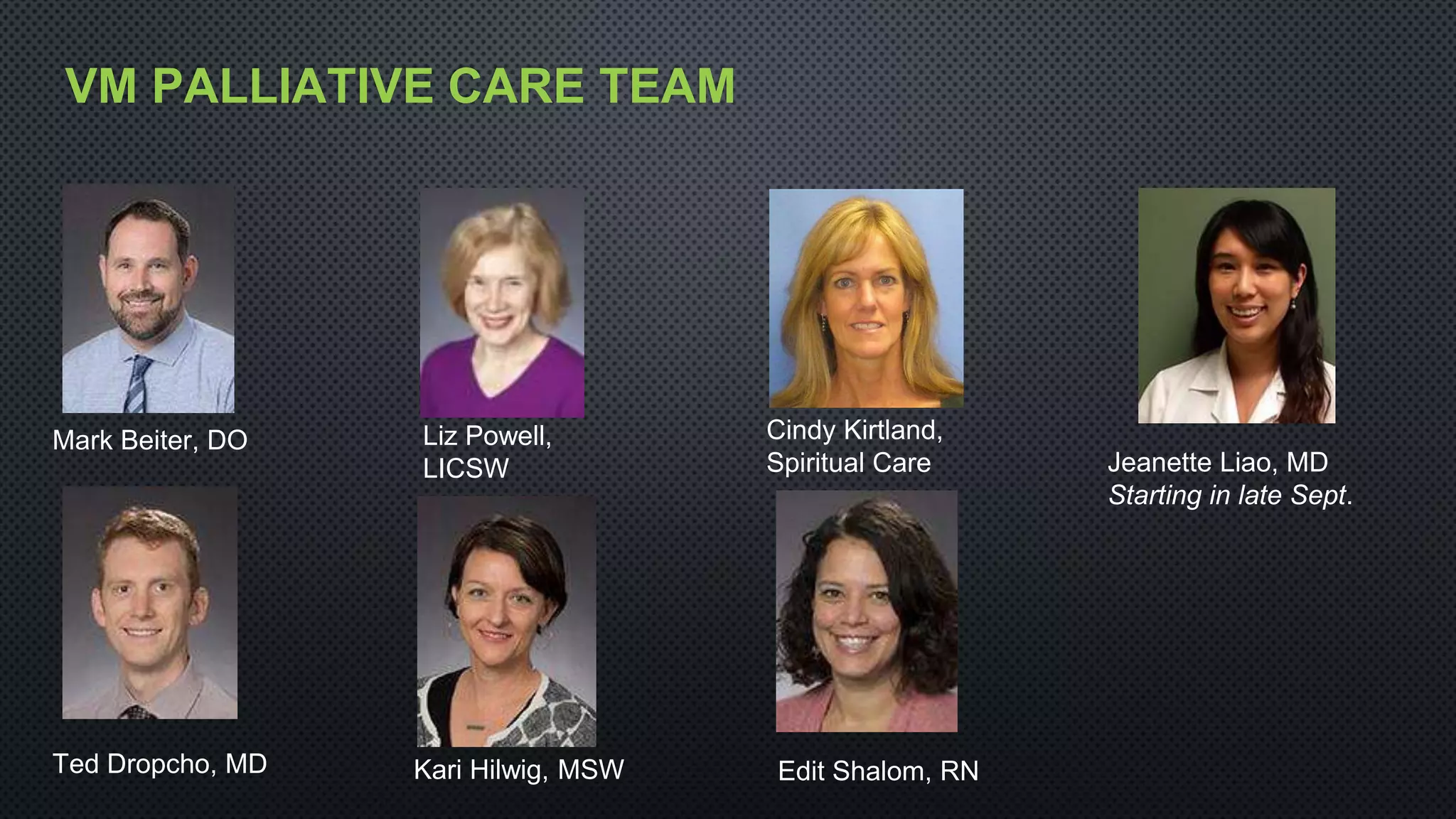
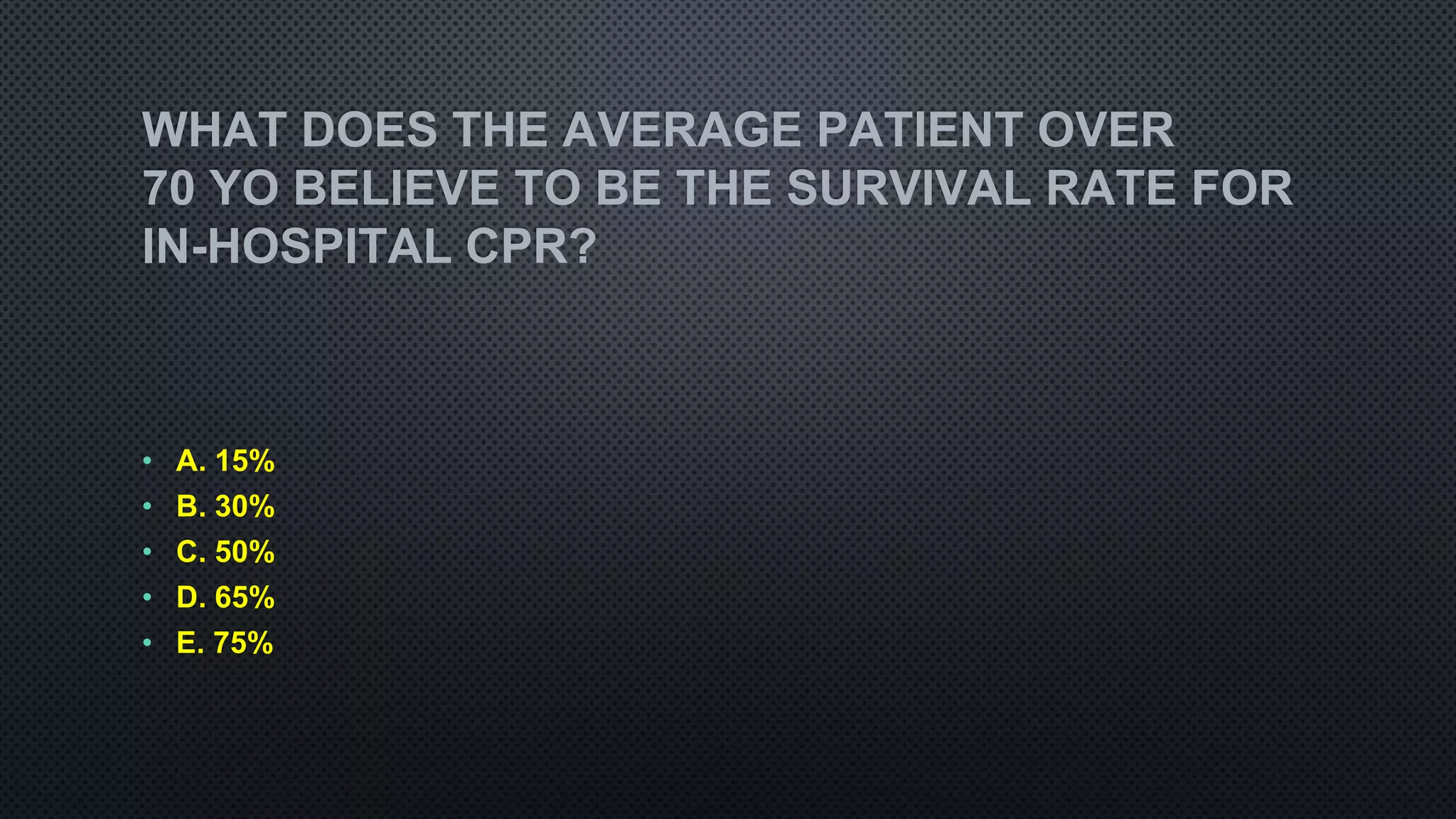

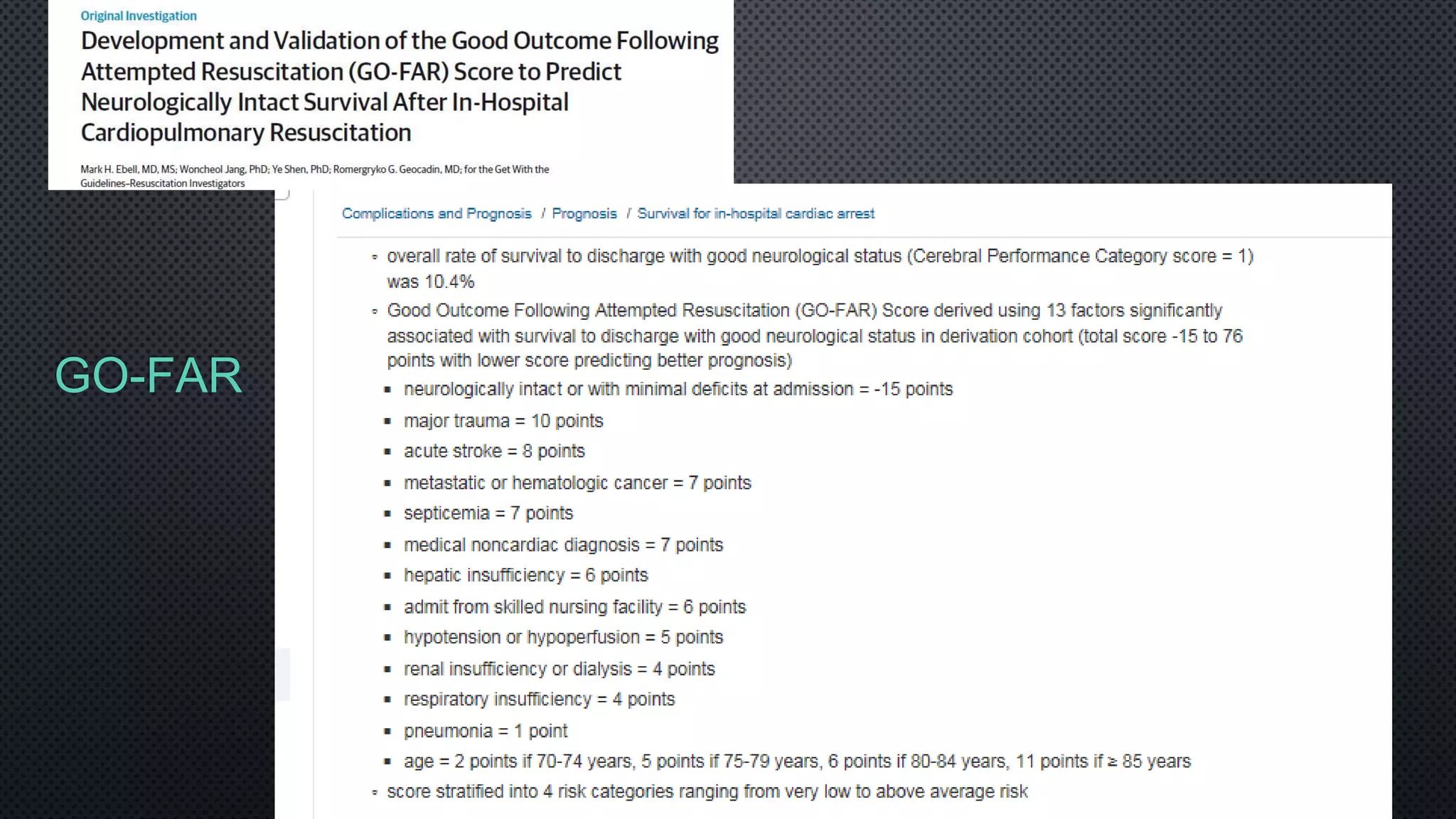
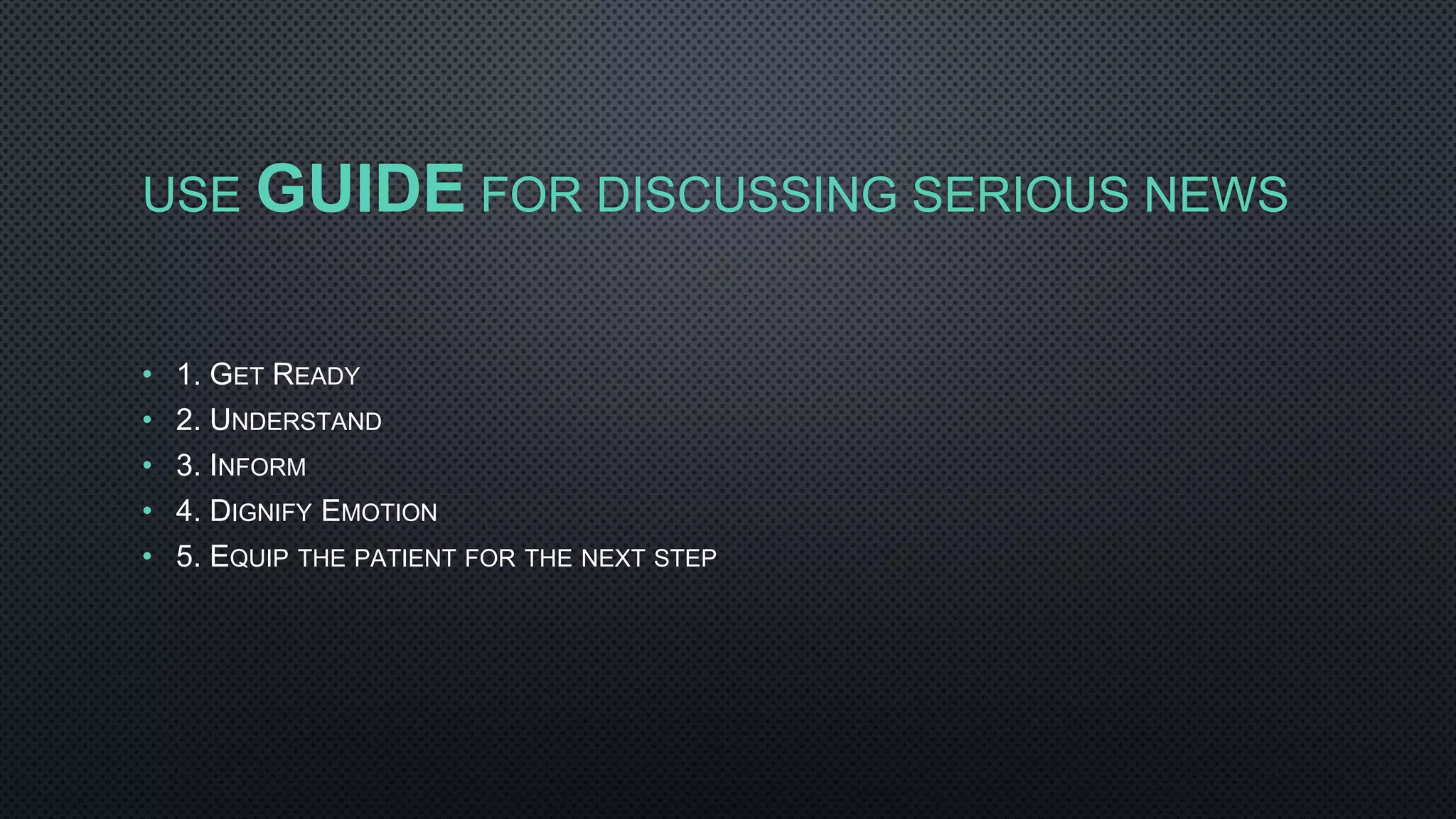
![DNR VS DNAR
• DNR IS MISLEADING AS IT IMPLIES THAT CPR IS ALWAYS POSSIBLE &
SUCCESSFUL. SO, IF YOU CHOOSE DNR, YOU CHOOSE TO FORGO A
SUCCESSFUL INTERVENTION.
• DNAR [DO NOT ATTEMPT RESUSCITATION] IS MORE ACCURATE AS IT
INDICATES THAT NO EFFORT WILL BE MADE TO ATTEMPT AN INTERVENTION
THAT HAS A LOW RATE OF SUCCESS FOR PATIENTS REACHING THE END OF
THEIR LIVES.](https://image.slidesharecdn.com/noonconfcodestatus-180710165731/75/Noon-conf-code-status-21-2048.jpg)
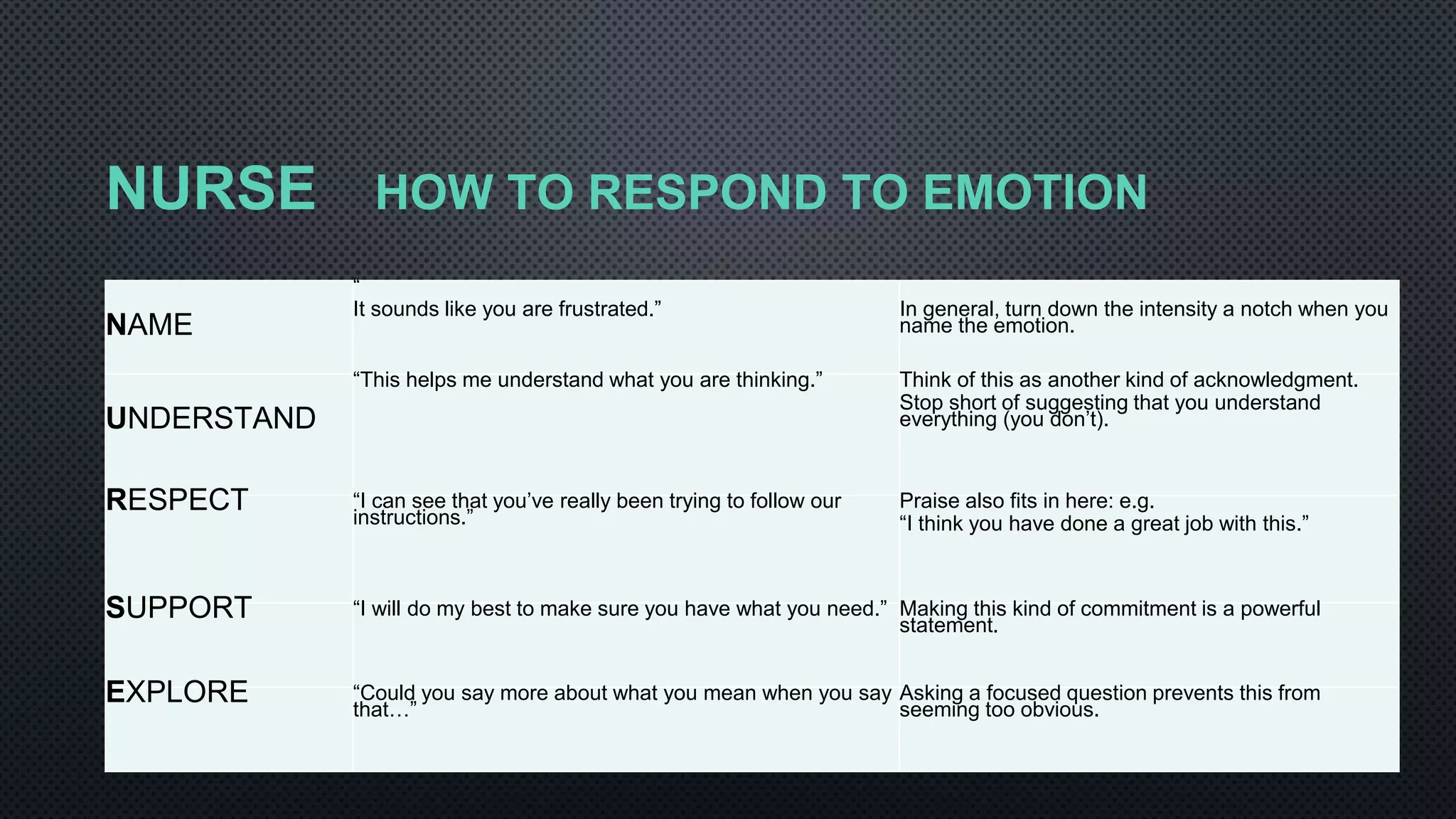
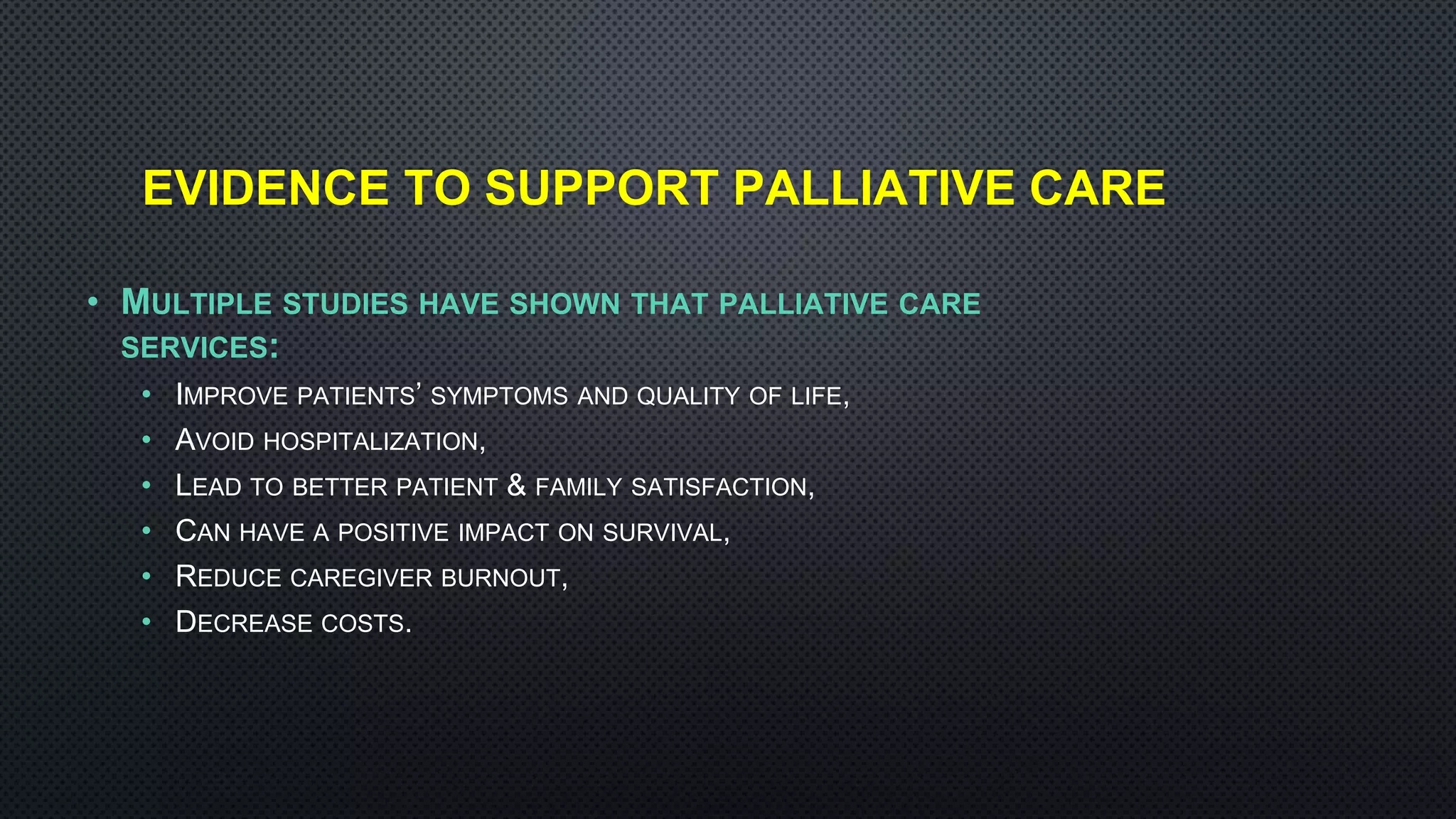
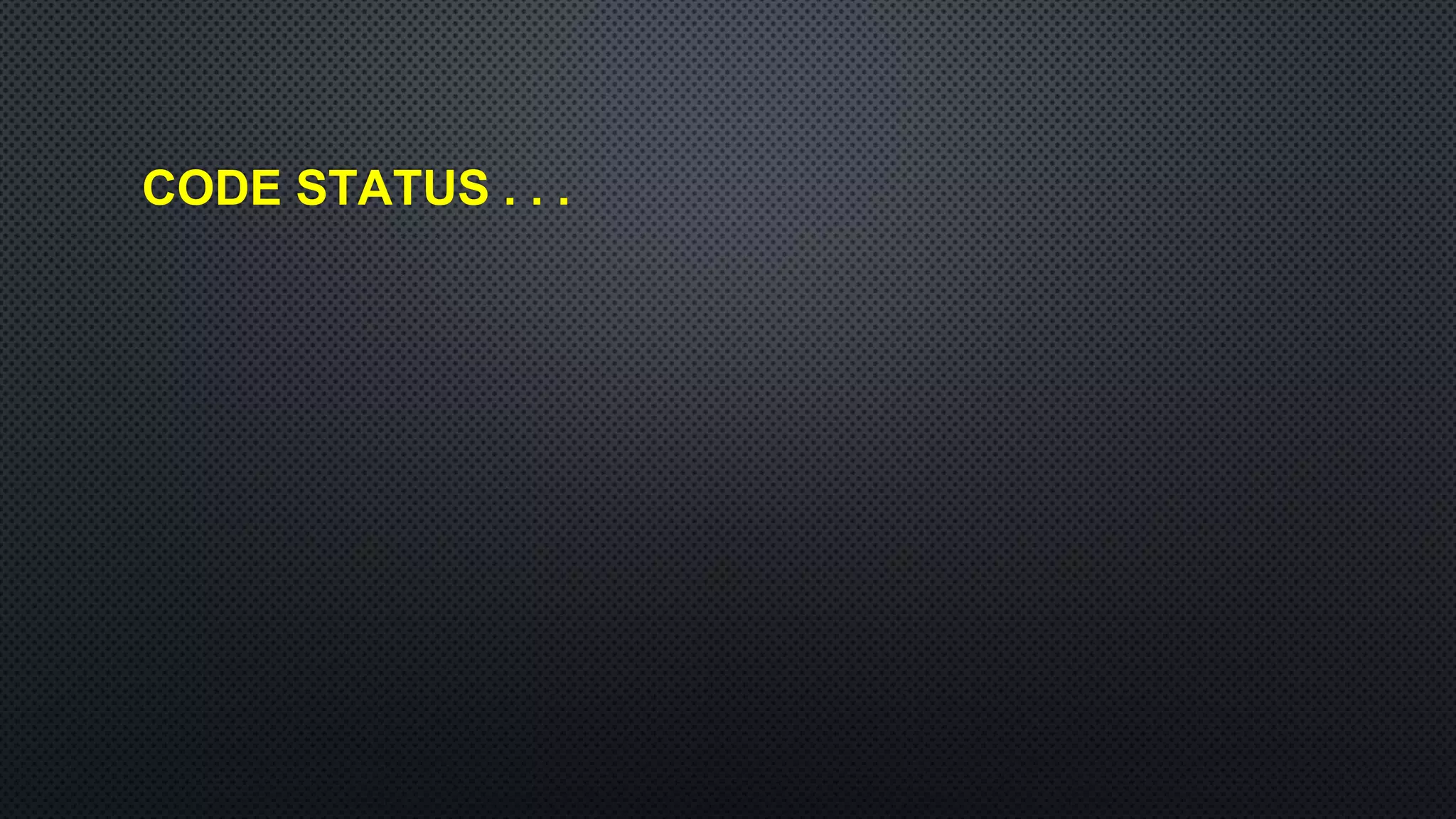
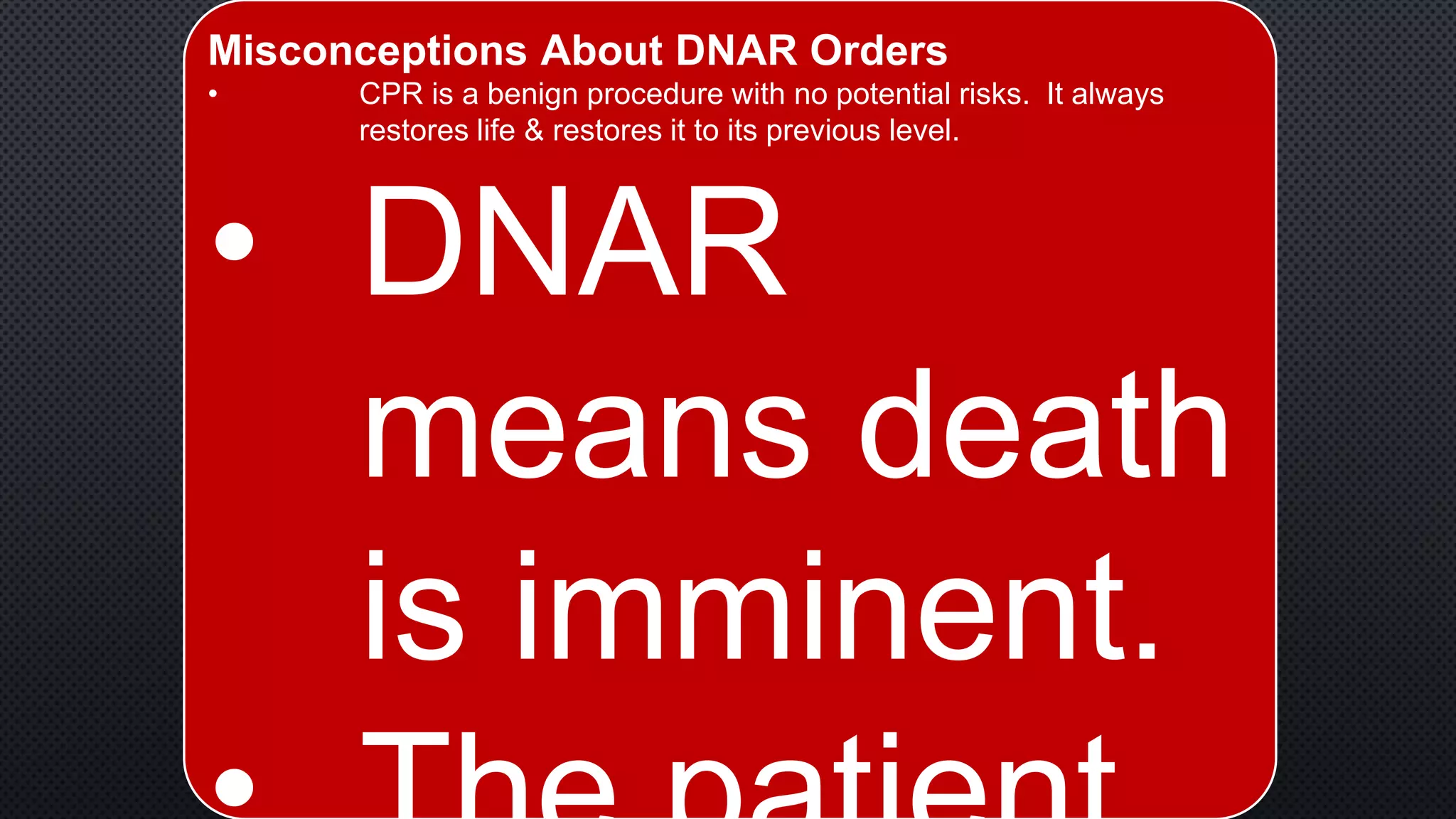
![CURRENT STATE:
• DNAR DISCUSSIONS HAPPEN TOO LITTLE & TOO LATE.
• MAJORITY OF DNAR ORDERS WRITTEN WITHIN 2-3 DAYS BEFORE DEATH.
• 500 PTS WHO SUFFERED CARDIAC ARREST, 76% OF THESE PTS WITH DNAR
ORDERS WERE INCAPACITATED AT THE TIME DNAR ORDER DISCUSSED. [ONLY
11% WERE IMPAIRED AT ADMISSION]. [BEDELL ET AL, JAMA 1986]
• DNAR DISCUSSIONS FAIL TO SATISFY INFORMED CONSENT.
• RARELY DO WE DISCUSS THE PATIENT’S GOALS, EXPLAIN THE CHANCES FOR
SURVIVAL, THE ASSOCIATED HARMS, AND THE ALTERNATIVES.
• HEALTH CARE PROFESSIONALS INAPPROPRIATELY EXTRAPOLATE
DNAR ORDERS TO OTHER DECISIONS.
• SURVEY OF 155 RESIDENTS: 43% WOULD WITHHOLD BLOOD PRODUCTS & 32%
WOULD NOT GIVE ANTIBIOTICS AFTER MAKING SOMEONE DNAR. [ARCH INTERN MED.
1988]](https://image.slidesharecdn.com/noonconfcodestatus-180710165731/75/Noon-conf-code-status-22-2048.jpg)
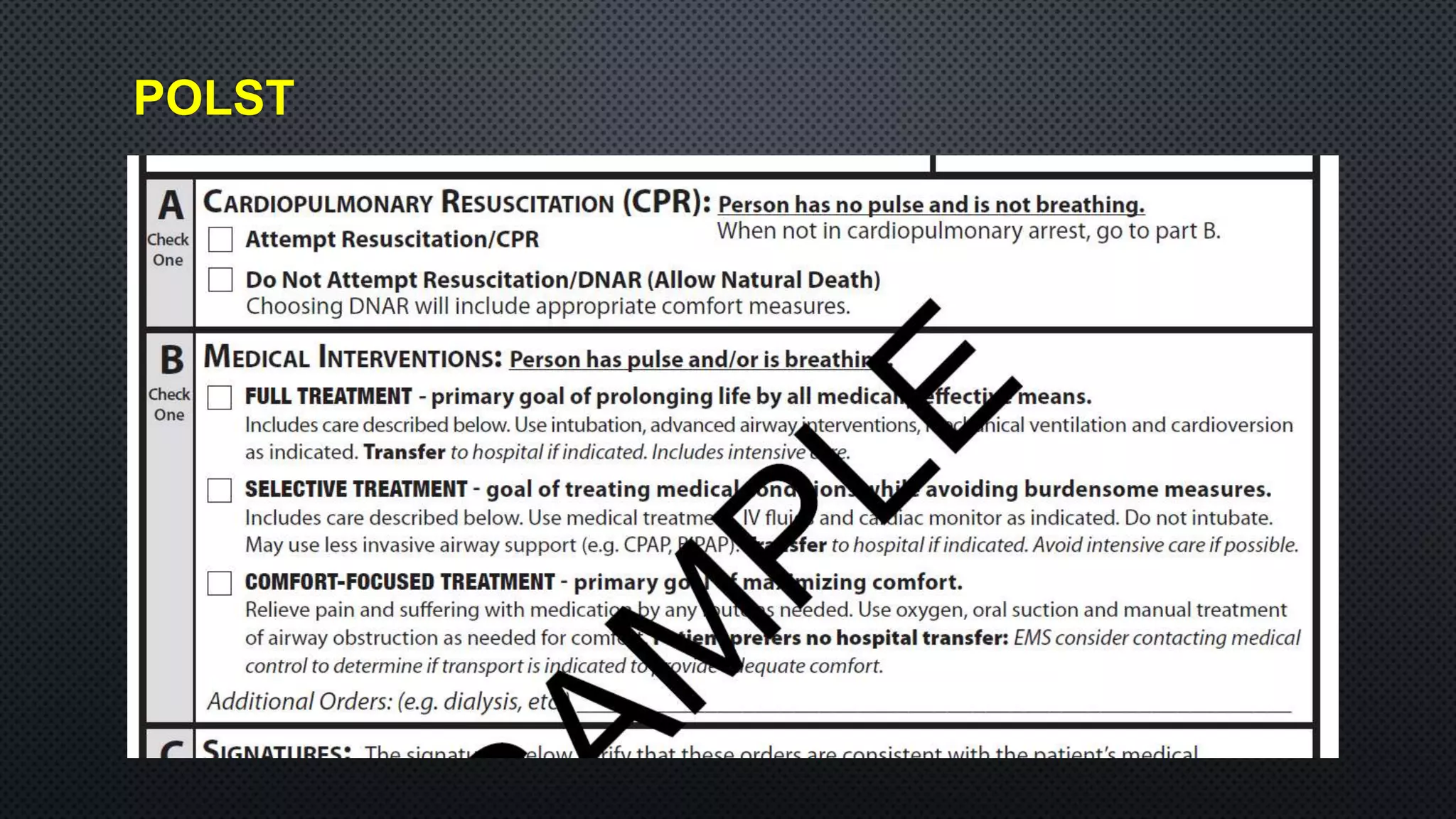
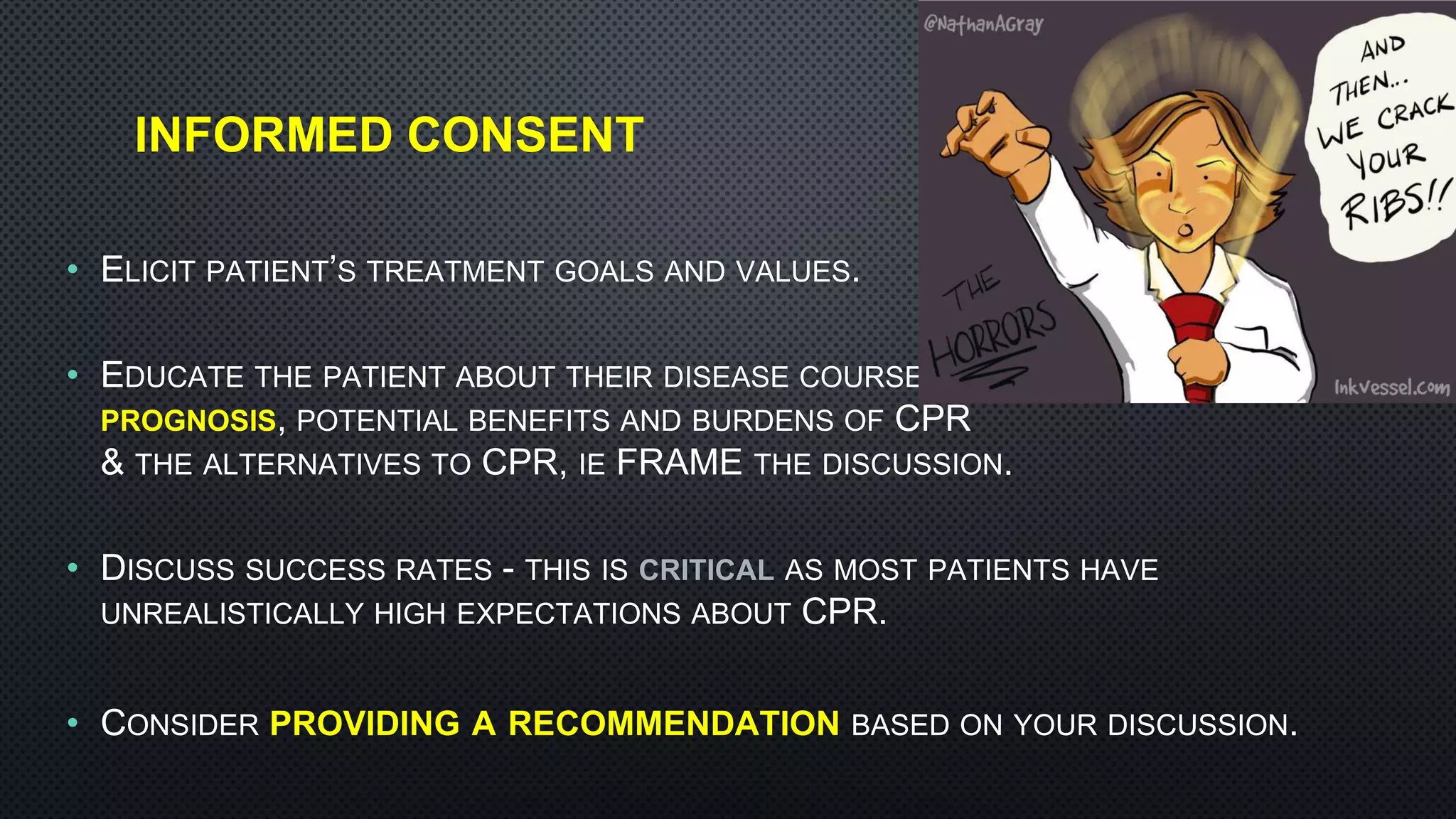
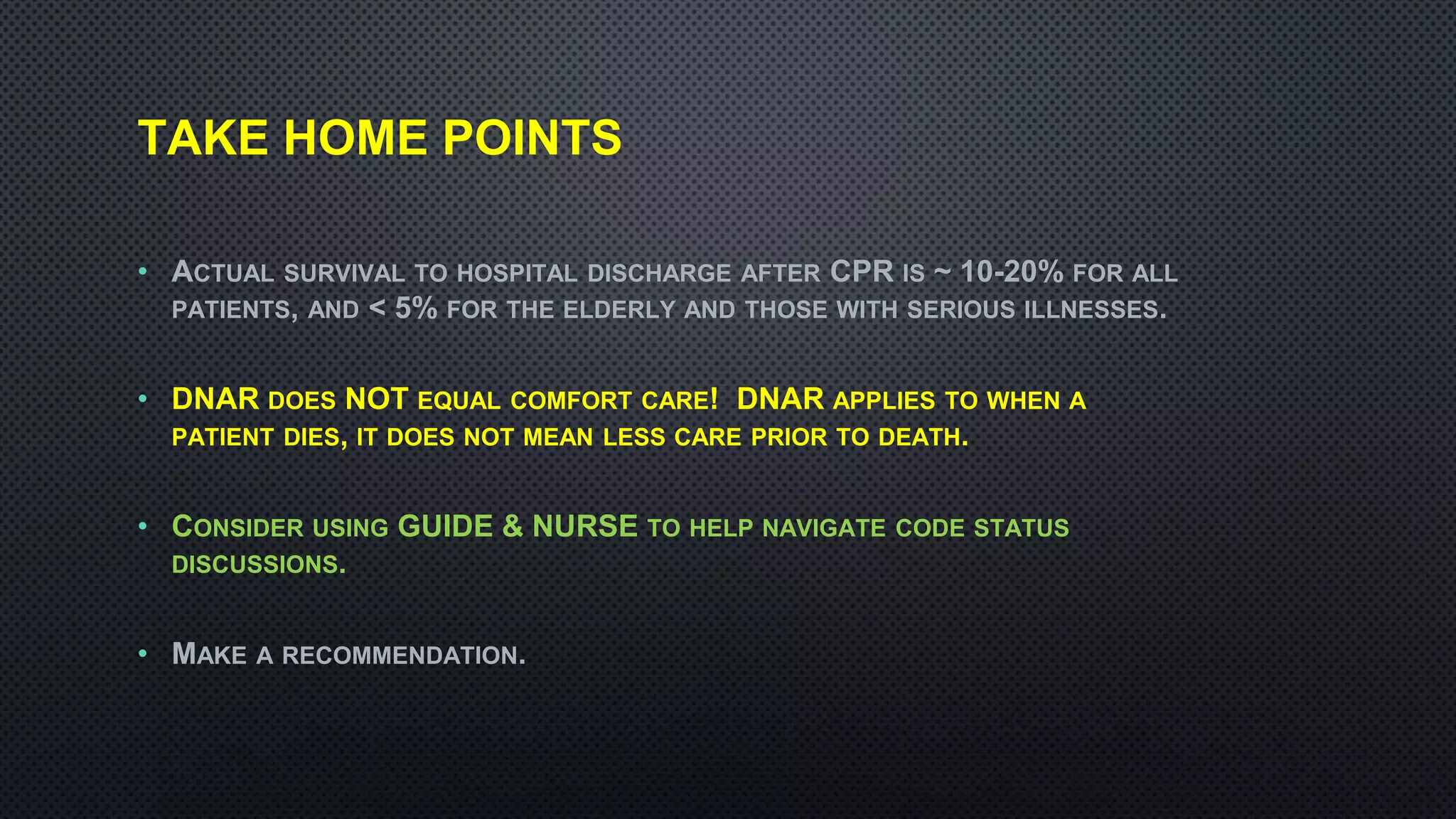
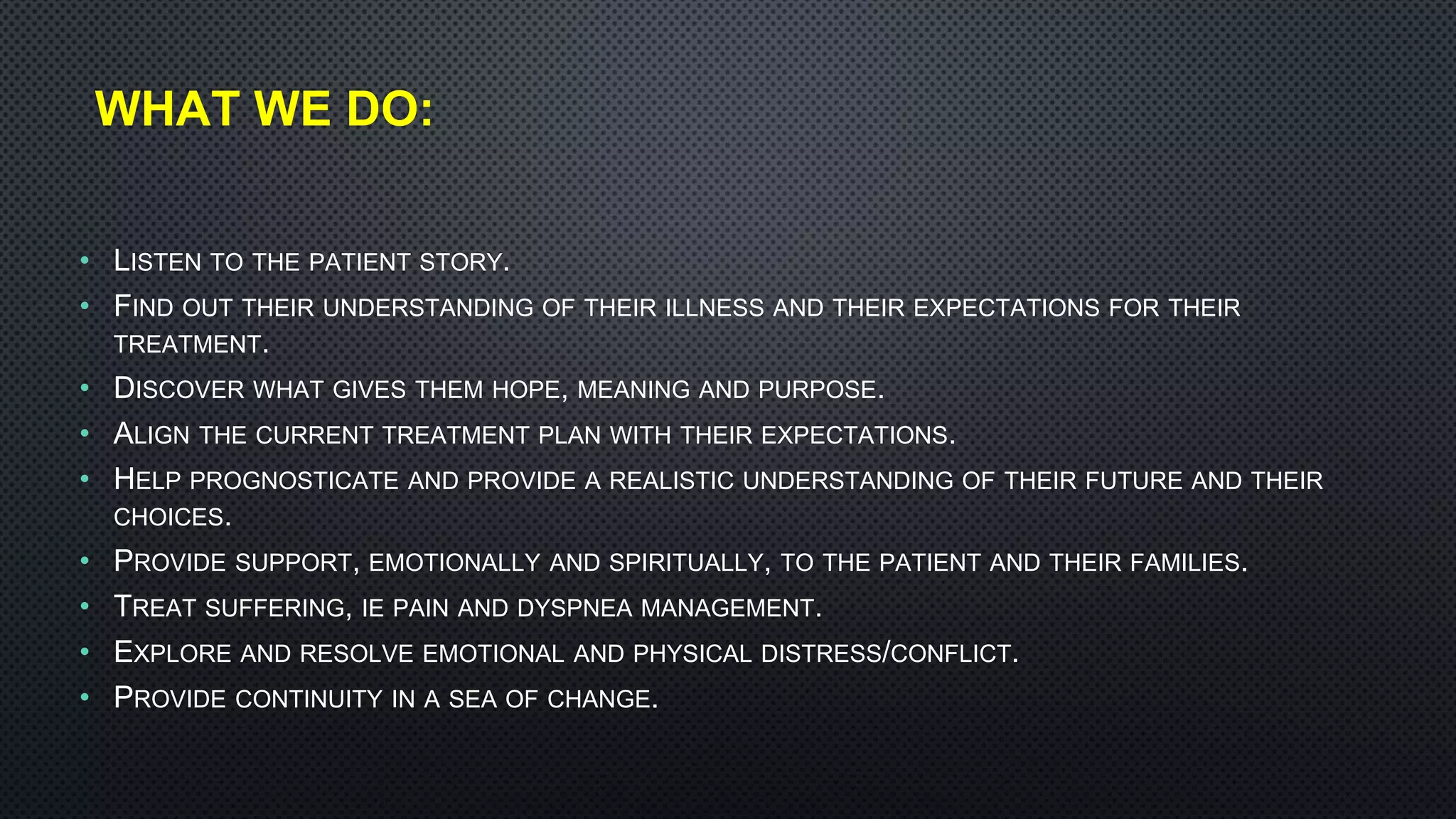
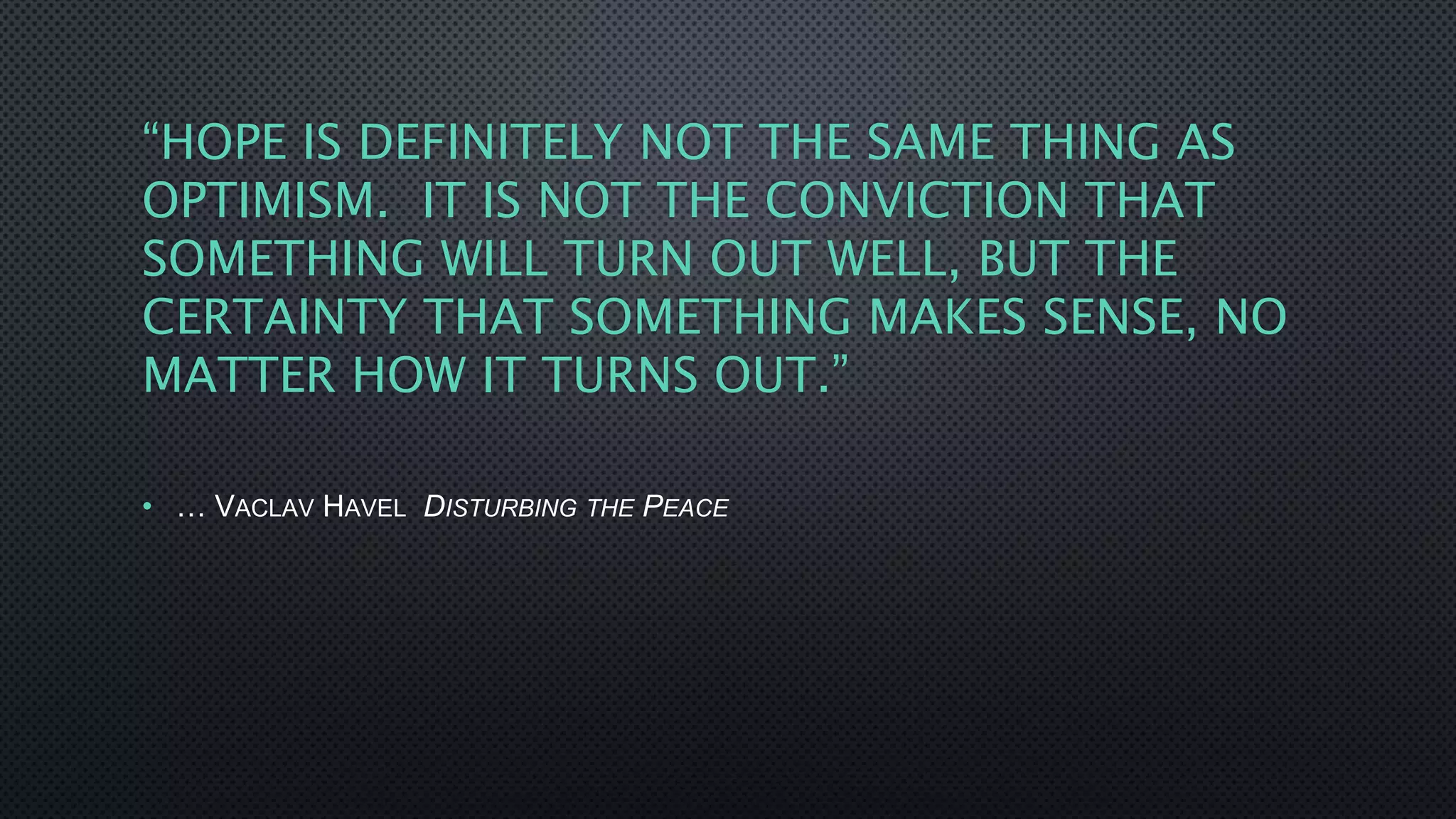
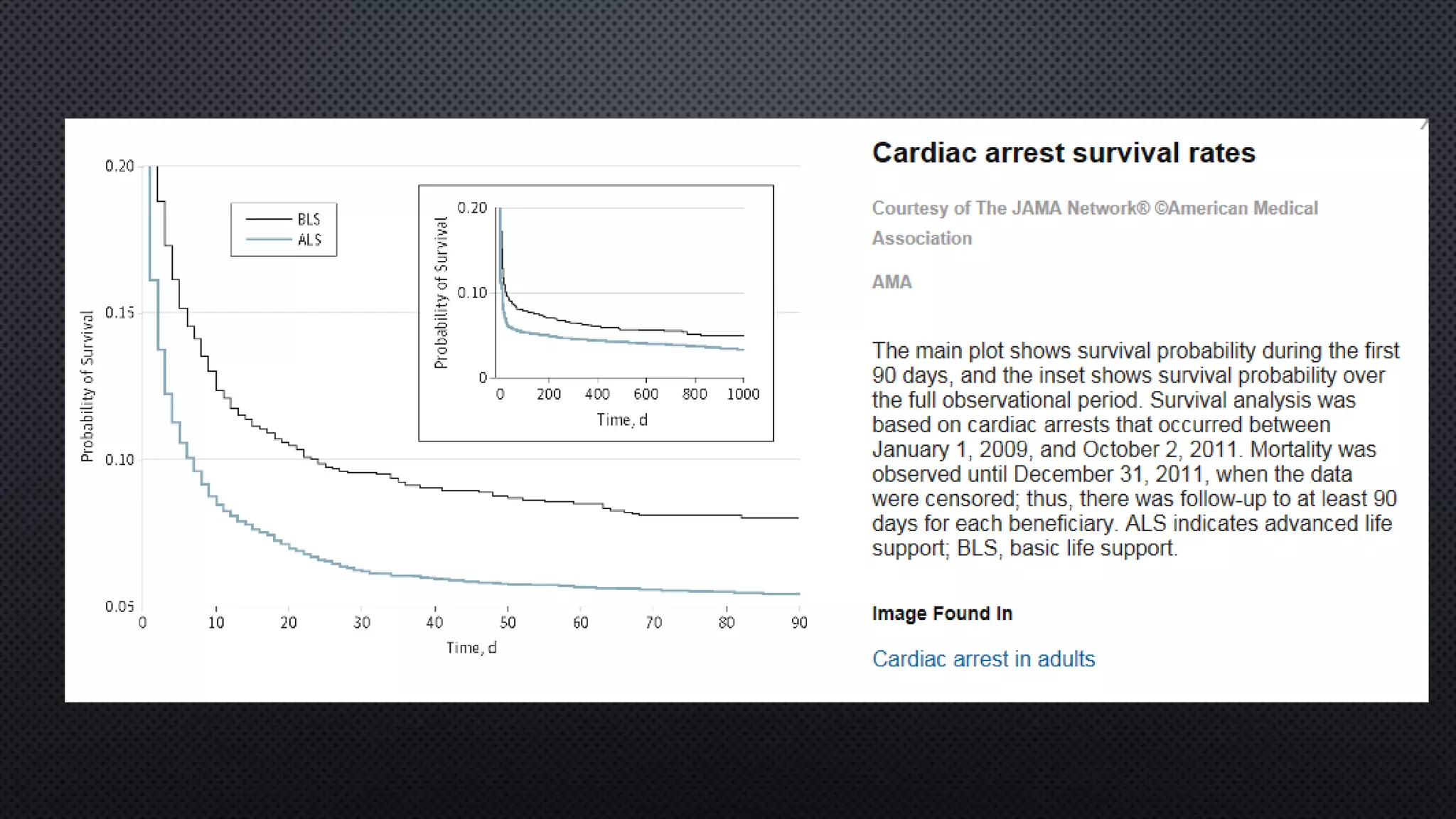
![SURVIVAL STATISTICS [IN-HOSPITAL ARREST]
Variable % survival at discharge
Overall average 17.5%
Age >75 1.3%
Age > 90 0.1% [n=576 pts]
Any Malignancy 6.6%
Stage IV malignancy 1.9%
Impaired renal function [any] 8%
Diabetes 11.7%
COPD 12%
One active diagnosis 21%
Primary diagnosis of CV disease 23%
Prior good health 27%
Arrhythmia 50%
CPR success rate on TV 64% [NEJM 1996]
From:
Ebell and Afonso.
Pre-arrest
predictors of
failure to survive
after in-hospital
CPR: a meta-
analysis. Family
Practice (2011)
28 (5): 505-515.
Meta-analysis of
35 studies with
96,499 pts.](https://image.slidesharecdn.com/noonconfcodestatus-180710165731/75/Noon-conf-code-status-25-2048.jpg)