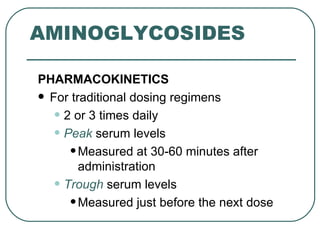
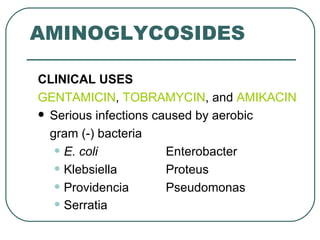
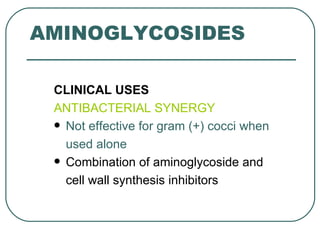
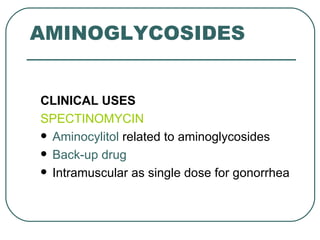
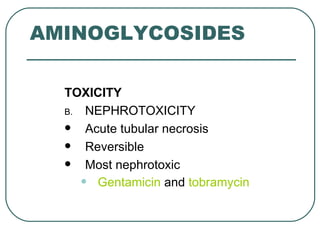
This document discusses aminoglycosides, a class of antibiotics. It describes their modes of antibacterial action including being concentration and time dependent, having a post-antibiotic effect, and toxicity depending on plasma concentration over time. Common aminoglycosides like gentamicin and tobramycin are used to treat infections from various aerobic gram-negative bacteria. Their mechanisms of action and resistance are explained. The document also covers the clinical uses, toxicities including ototoxicity and nephrotoxicity, and precautions for aminoglycoside administration.