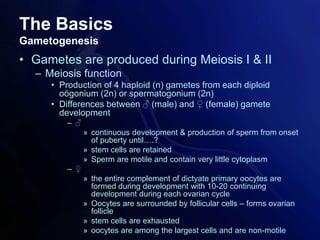
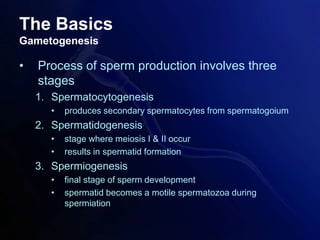
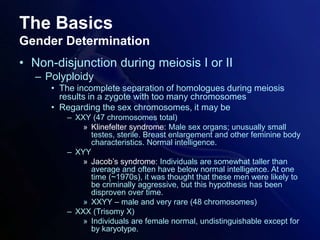
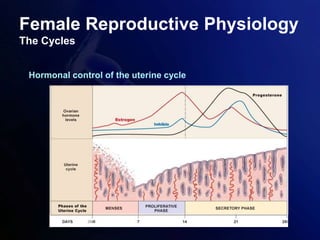
This document provides an outline for a lecture on reproductive physiology. It begins with an overview of gametogenesis and gender determination. It then discusses the pituitary-gonad axis and its role in regulating the reproductive cycles. Female reproductive physiology is examined, including the ovarian cycle, uterine cycle, and hormonal control of both cycles. Finally, it covers the basics of male reproductive physiology such as sperm production in the testes and the role of hormones.