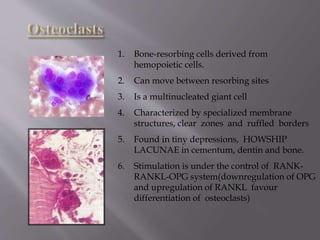
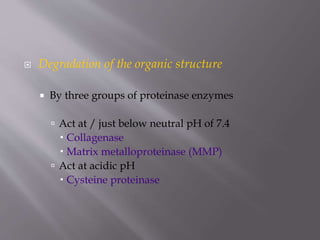
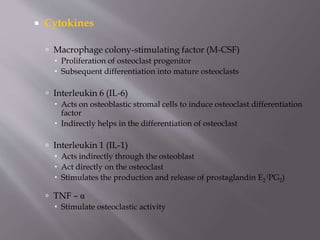
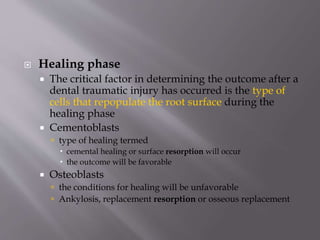
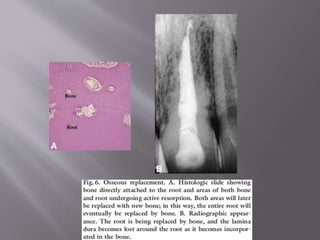
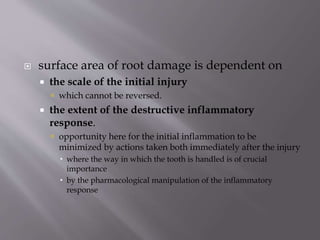
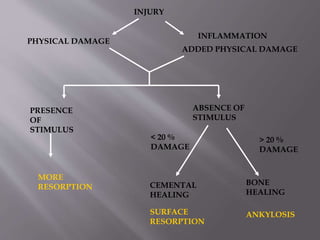
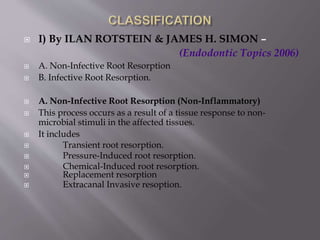
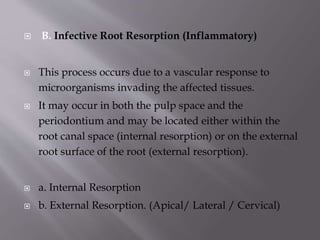
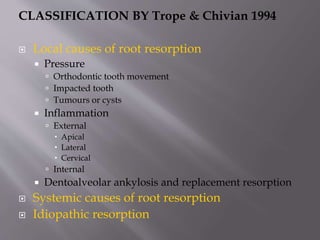
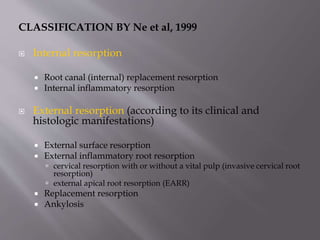
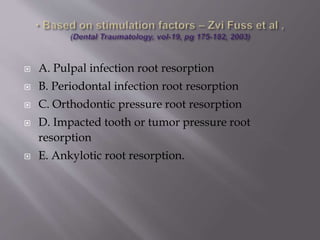
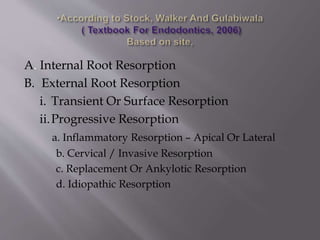
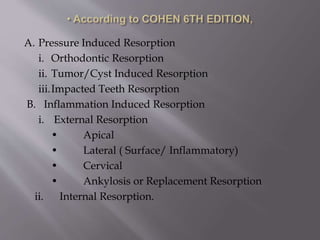
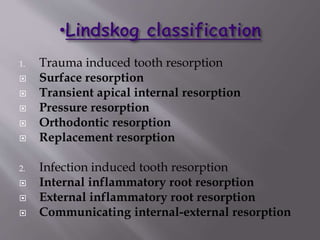
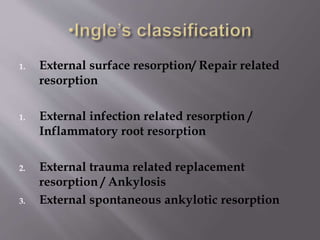
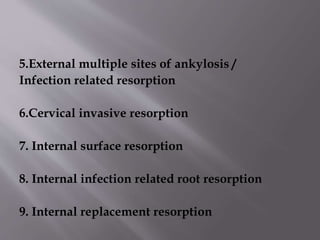
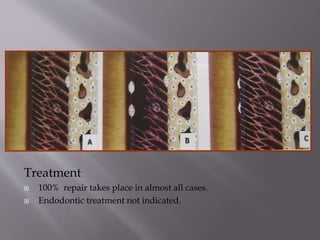
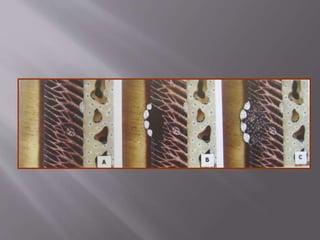
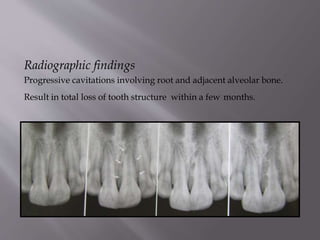
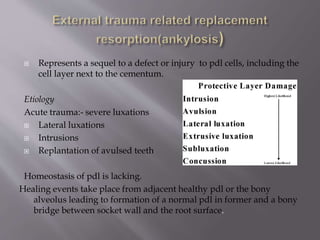
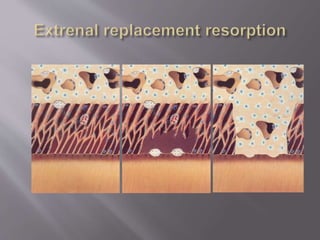
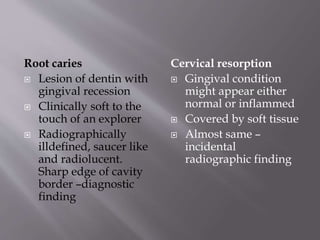
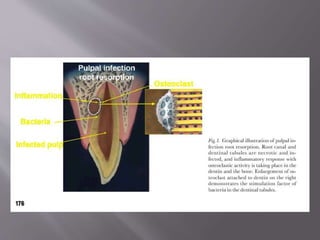
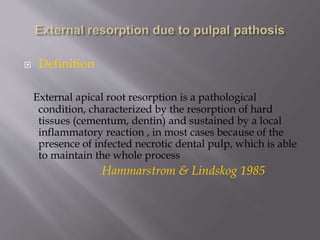
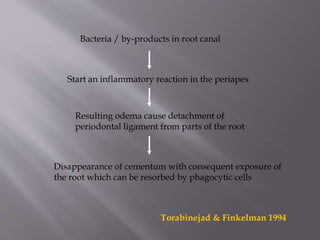
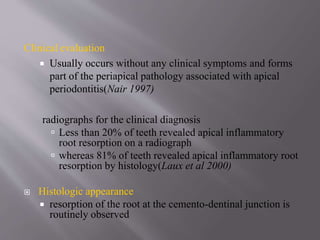
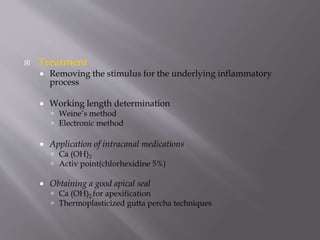
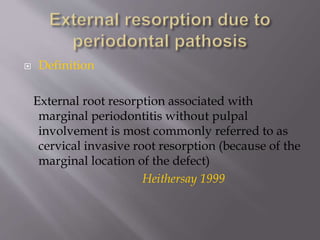
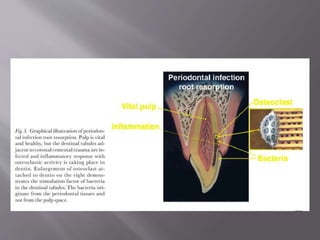
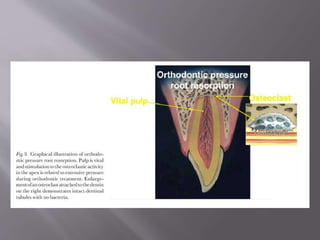
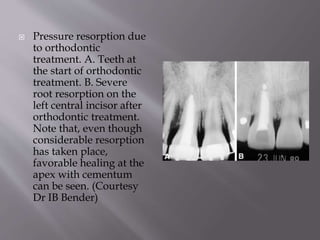
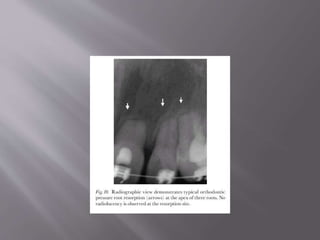
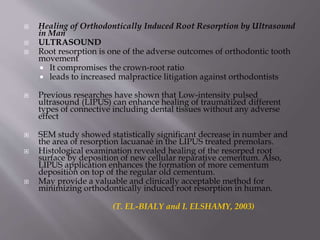
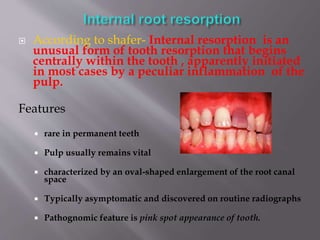
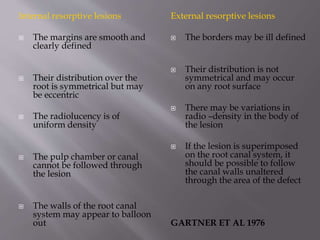
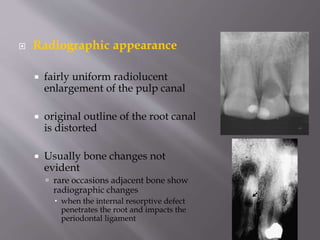
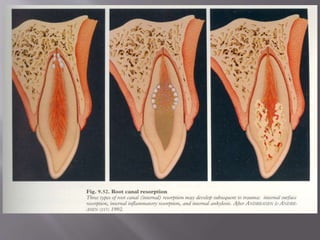
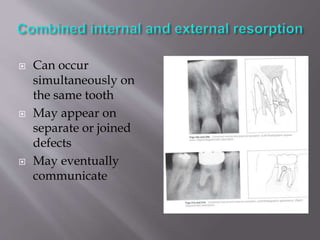
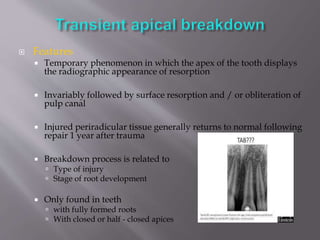
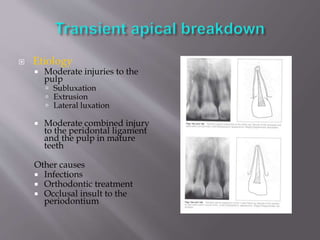
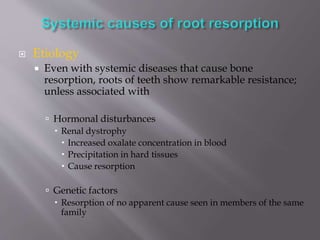
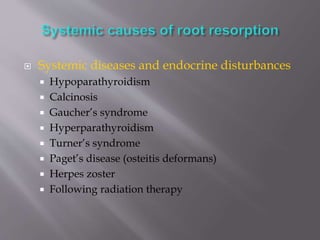
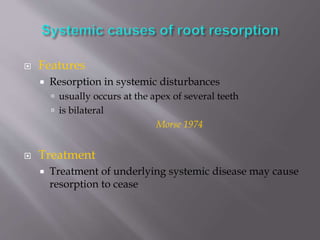
This document provides an overview of root resorption, including definitions, classifications, mechanisms, and types. It discusses physiological versus pathological root resorption and defines internal and external resorption. Key cells involved in the resorption process are osteoclasts and odontoclasts. Resorption requires inflammatory stimuli and occurs via acidification and enzymatic degradation. Factors like trauma, pressure, and infection can lead to resorption if they damage the protective root layers. The document classifies and describes various types of internal and external resorption.