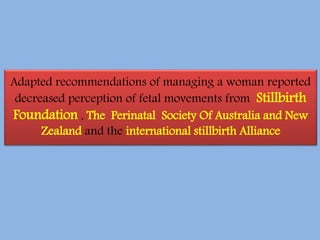
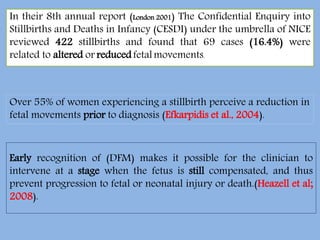
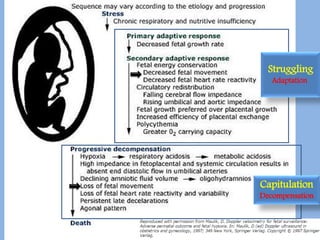
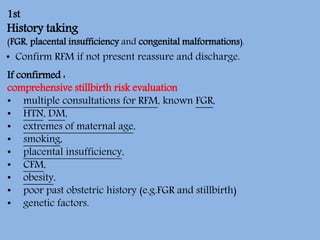
This document discusses decreased fetal movements (DFM) and provides guidance on evaluating and managing cases of reported DFM. Key points include:
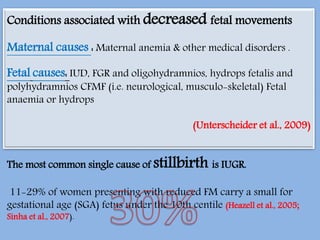
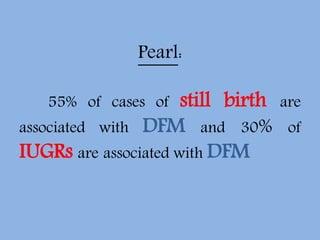
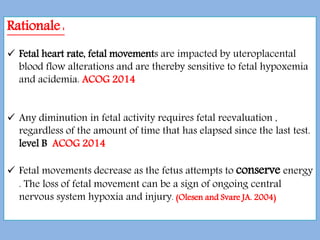
- DFM can be an early sign of fetal compromise and is associated with 16.4% of stillbirths.
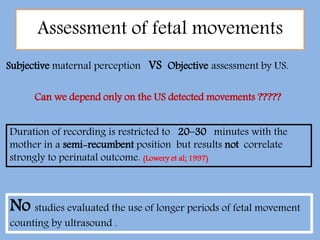
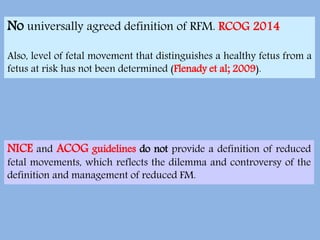
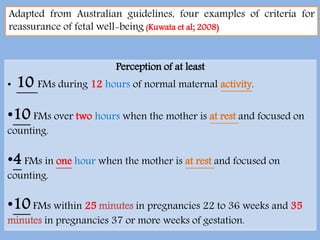
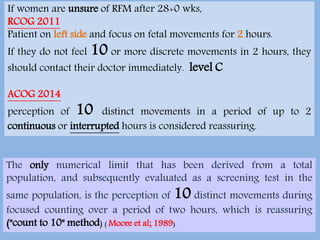
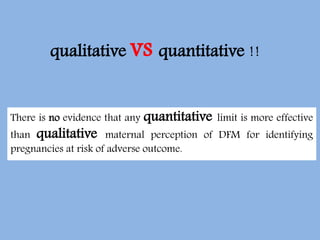
- There is no agreed upon definition of reduced fetal movements. Guidelines recommend focusing on qualitative maternal perception.
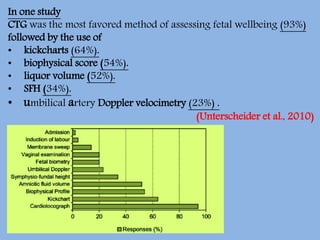
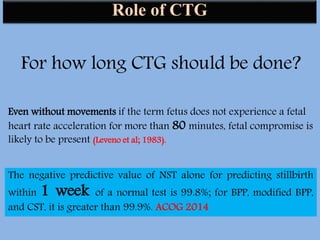
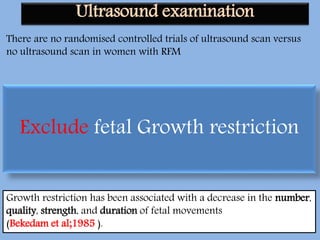
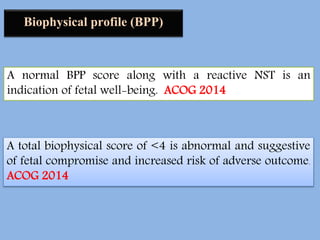
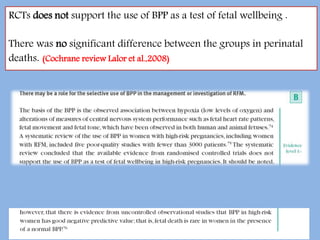
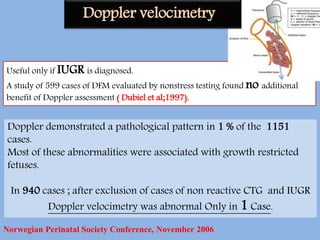
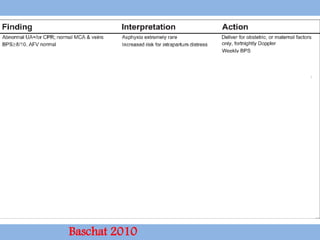
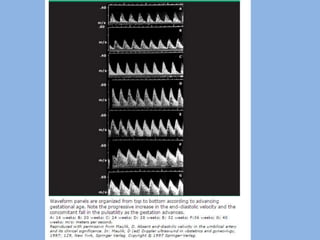
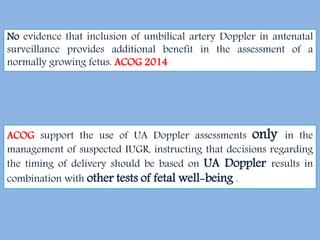
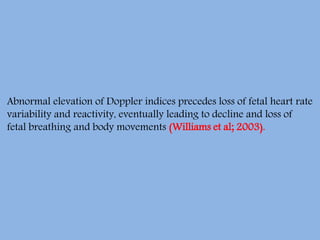
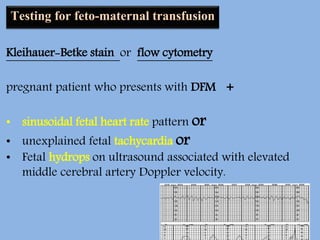
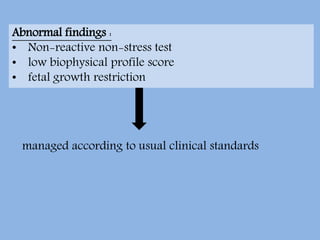
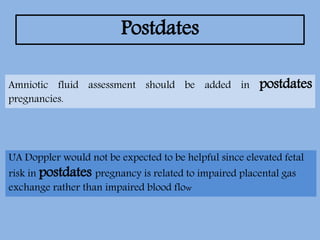
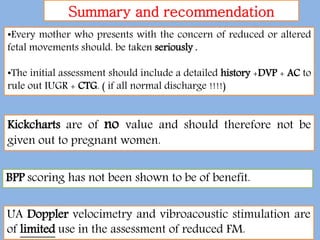
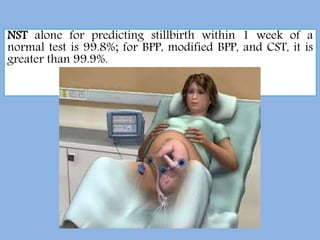
- Evaluation of DFM includes history, exam, NST, ultrasound to check growth, amniotic fluid and anatomy, and may include BPP, Doppler, biophysical profile if indicated.
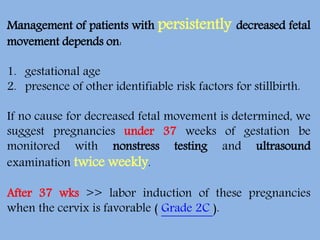
- For persistent unexplained DFM, monitoring with NST and ultrasound twice weekly is suggested under 37 weeks, induction after 37 weeks if cervix is


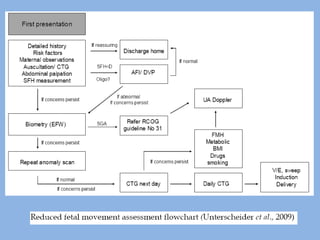
![Clinical approaches described in observational studies include:
1. physical examination including SFH
2. non-stress and contraction stress tests.
3. ultrasound examination (biophysical profile [BPP])
4. umbilical artery Doppler.
5. testing for fetomaternal hemorrhage (eg, Kleihauer-Betke test).
6. Amnioscopy.](https://image.slidesharecdn.com/decreasedfetalmovementsworkshop-170317152923/85/Decreased-fetal-movements-2017-31-320.jpg)