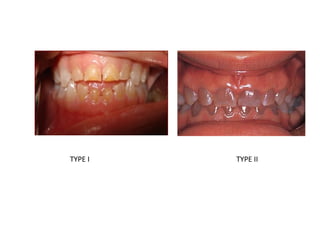
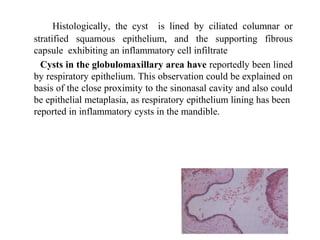
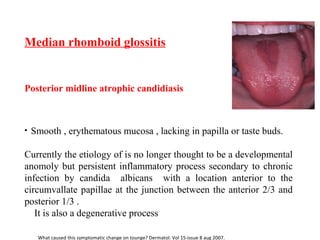
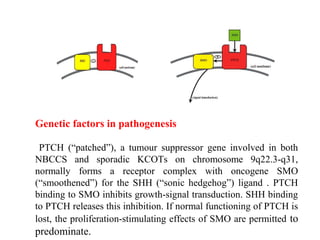
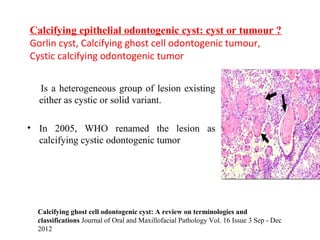
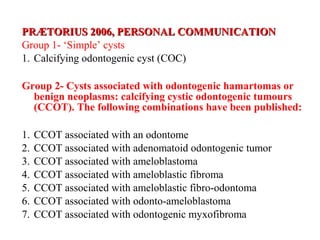
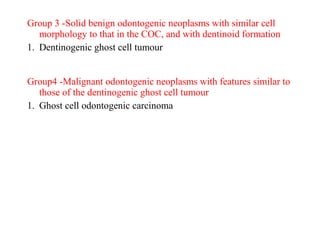
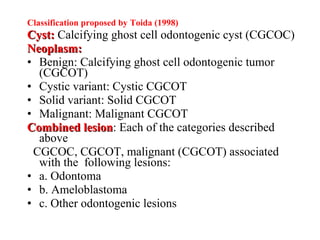
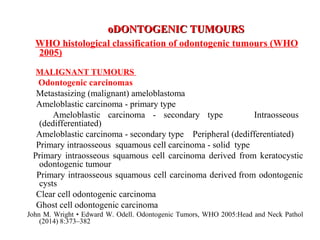
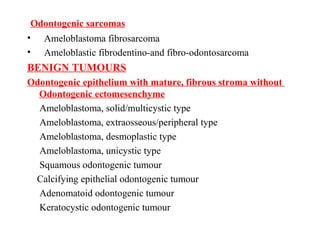
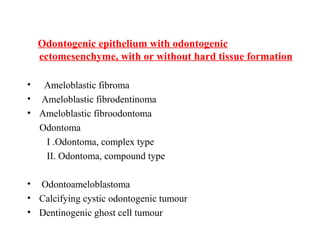
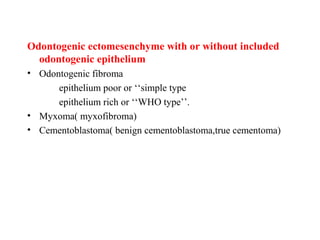
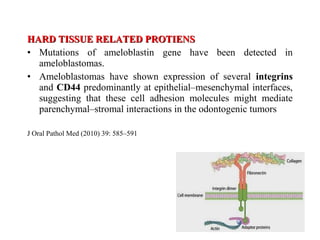
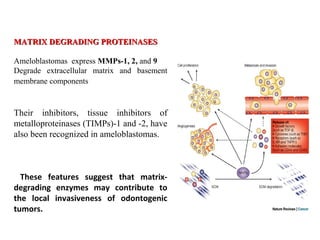
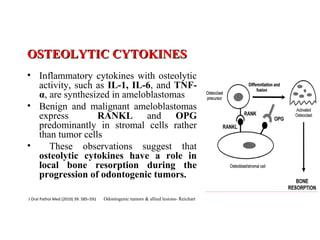
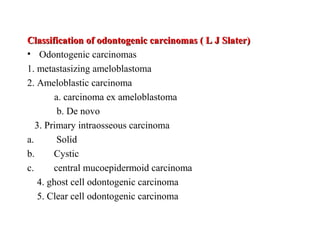
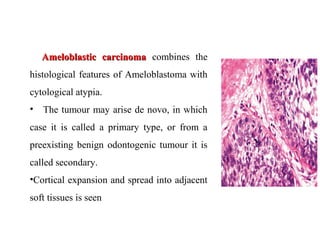
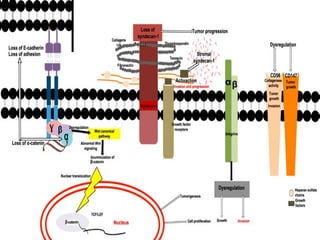
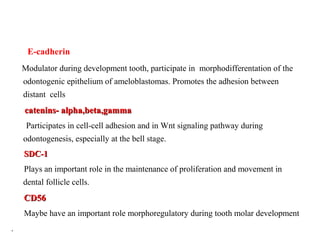
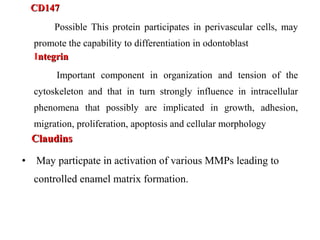
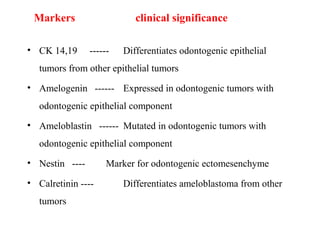
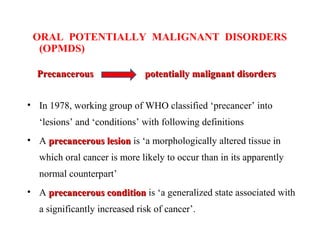
The document discusses recent concepts in developmental disturbances and odontogenic tumors, outlining classifications such as dentinogenesis imperfecta and the controversial globulomaxillary cyst. It explores the pathogenesis, histology, and molecular markers of various odontogenic tumors, including keratocystic odontogenic tumors and ameloblastomas. Additionally, it reviews the classification of benign and malignant tumors, emphasizing their characteristics and implications for diagnosis and treatment.