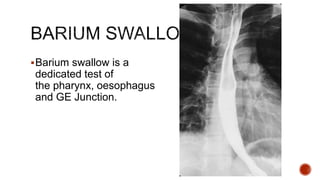
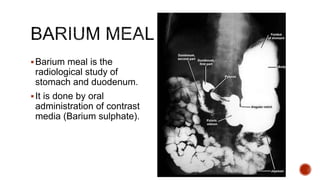
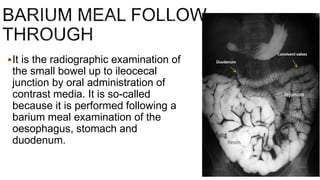
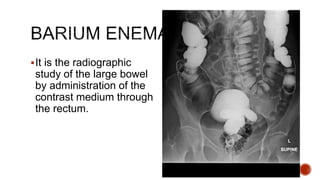
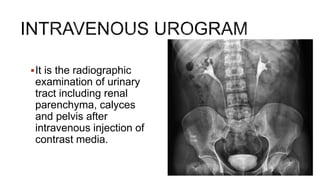
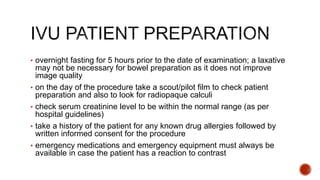
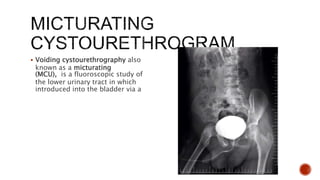
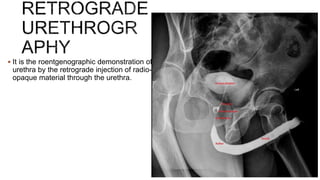
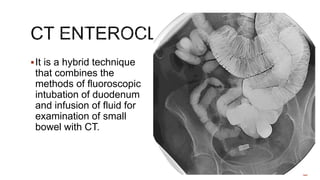
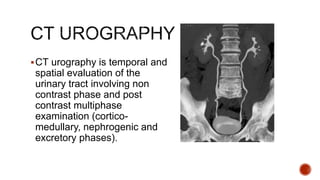
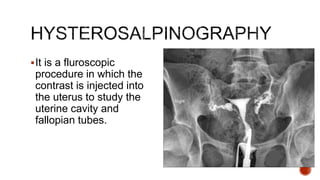
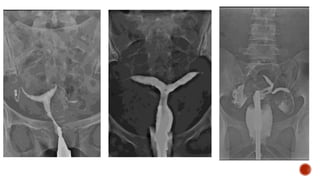
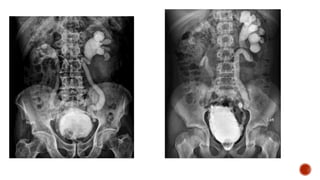
This document discusses various radiological procedures used to examine different parts of the body. It provides information on barium swallow, barium meal, small bowel follow through, barium enema, intravenous urogram, voiding cystourethrogram, retrograde urethrogram, CT enteroclysis, CT urography, hysterosalpingography and their clinical indications and patient preparation requirements.