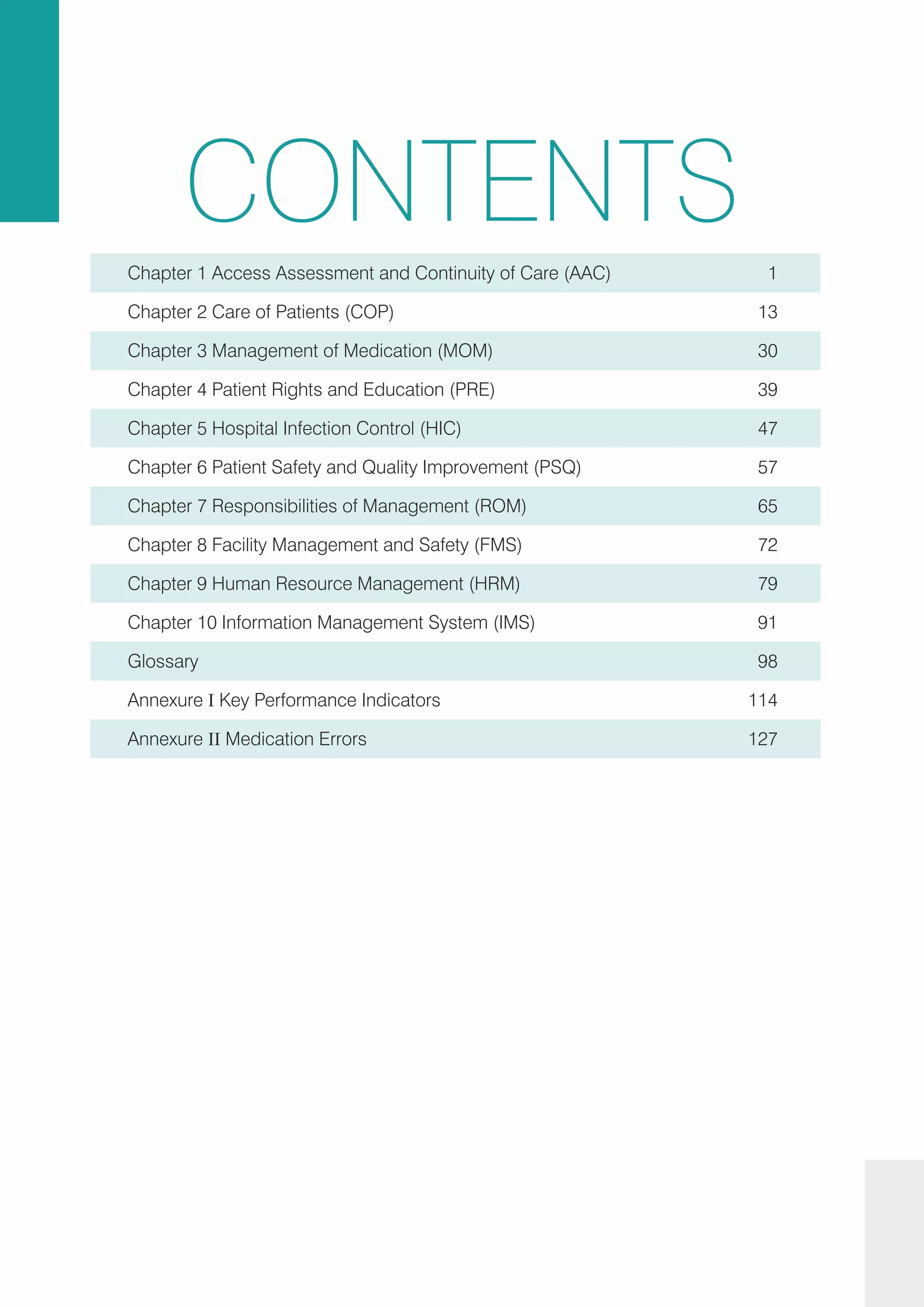
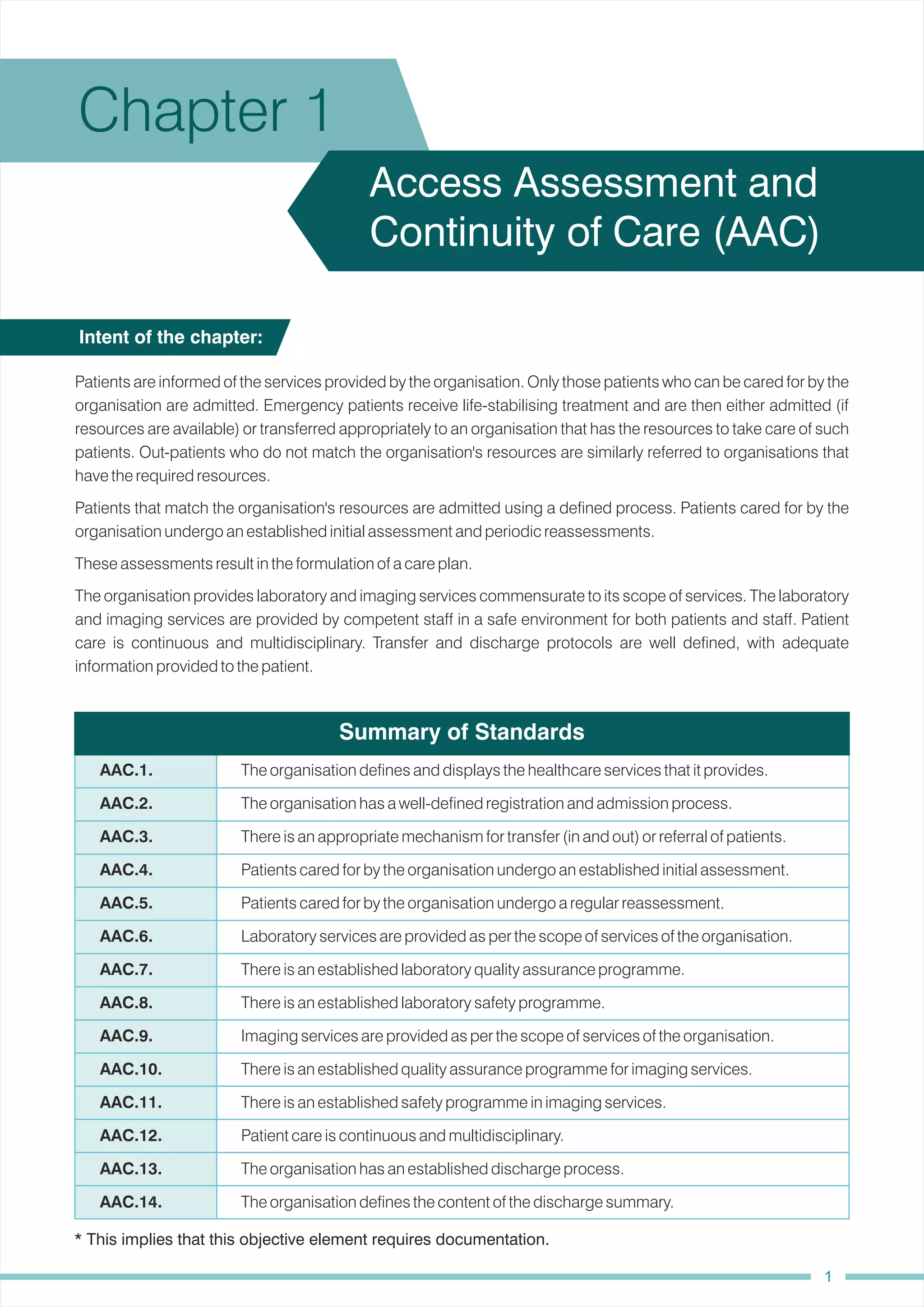
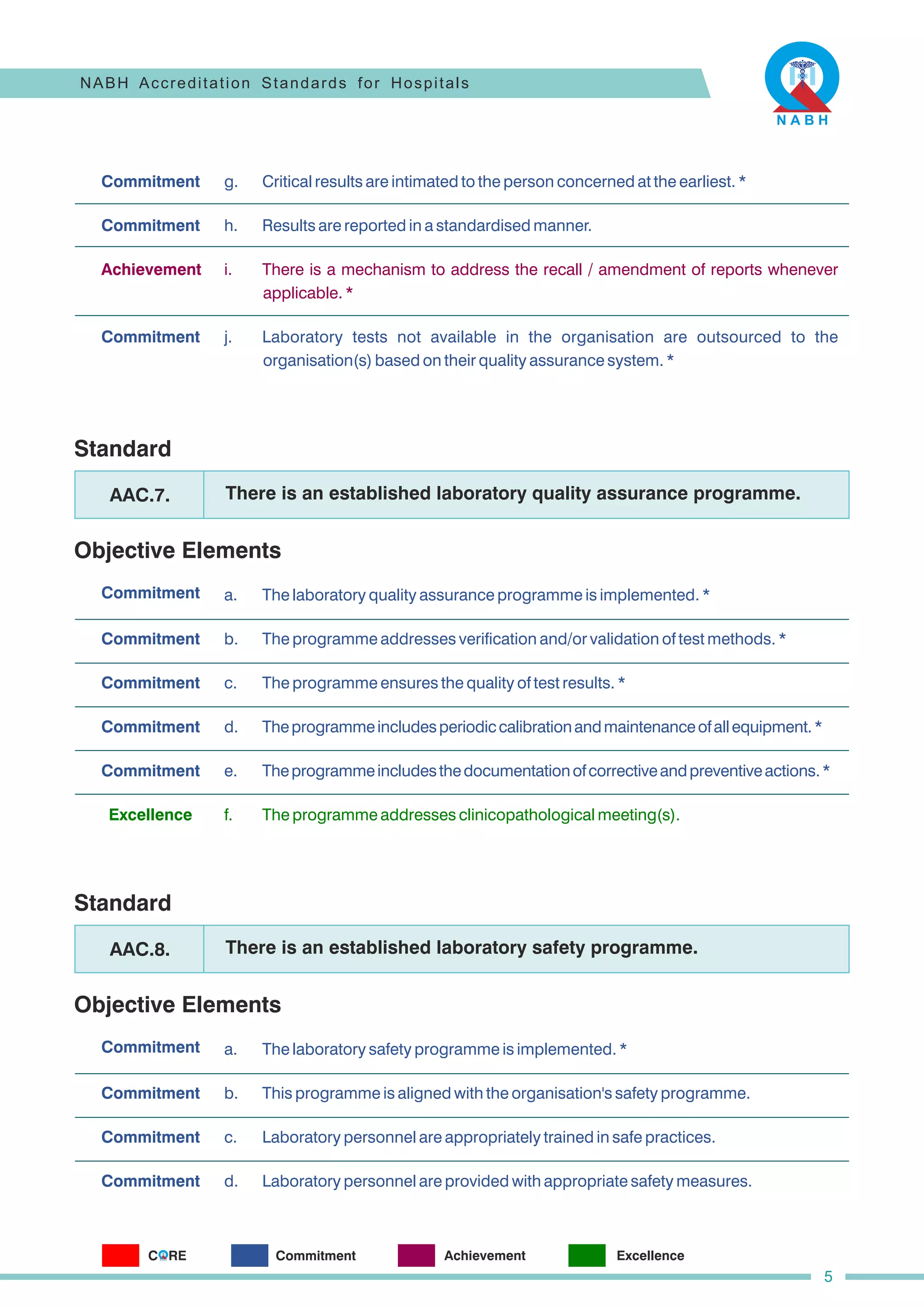
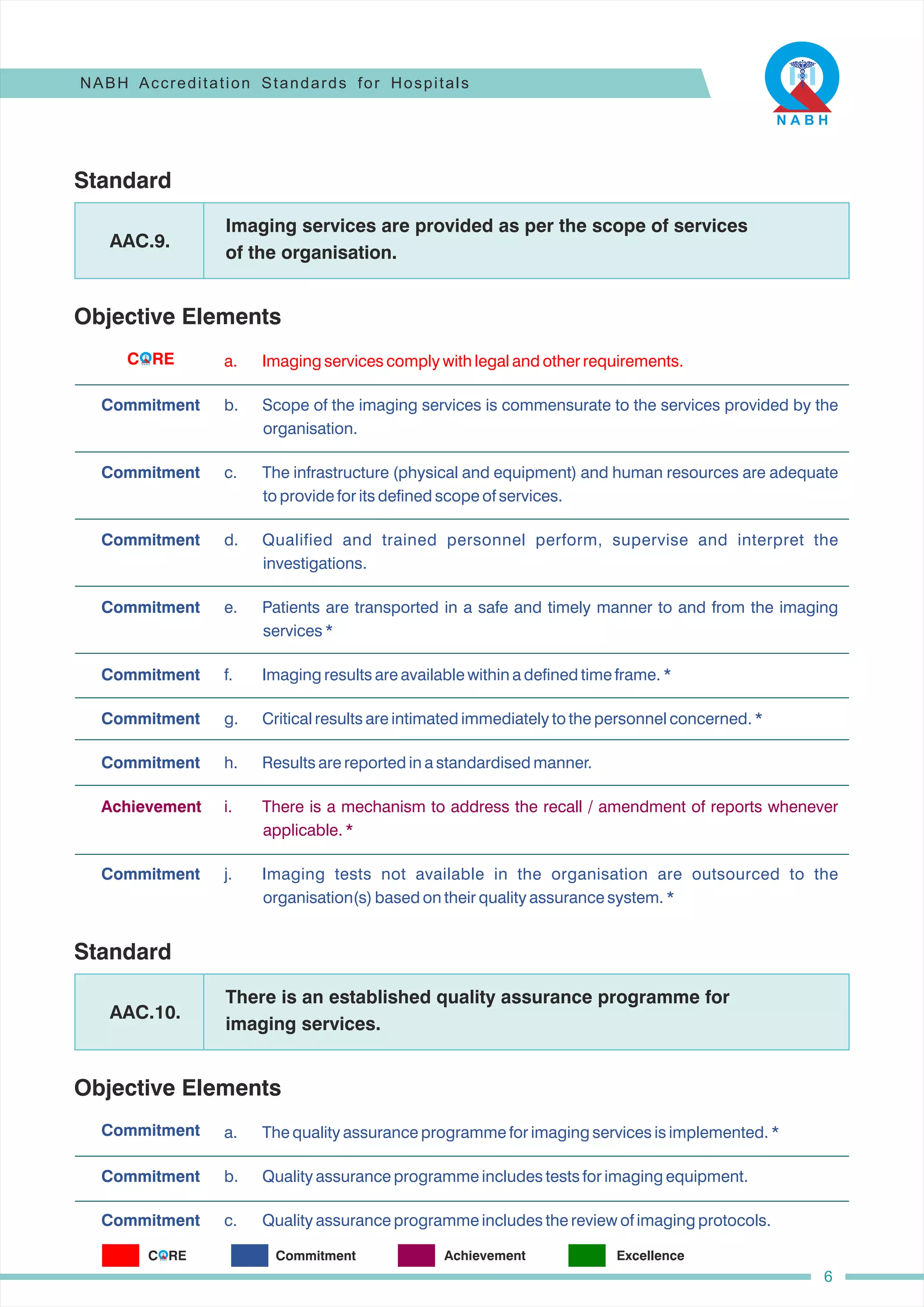
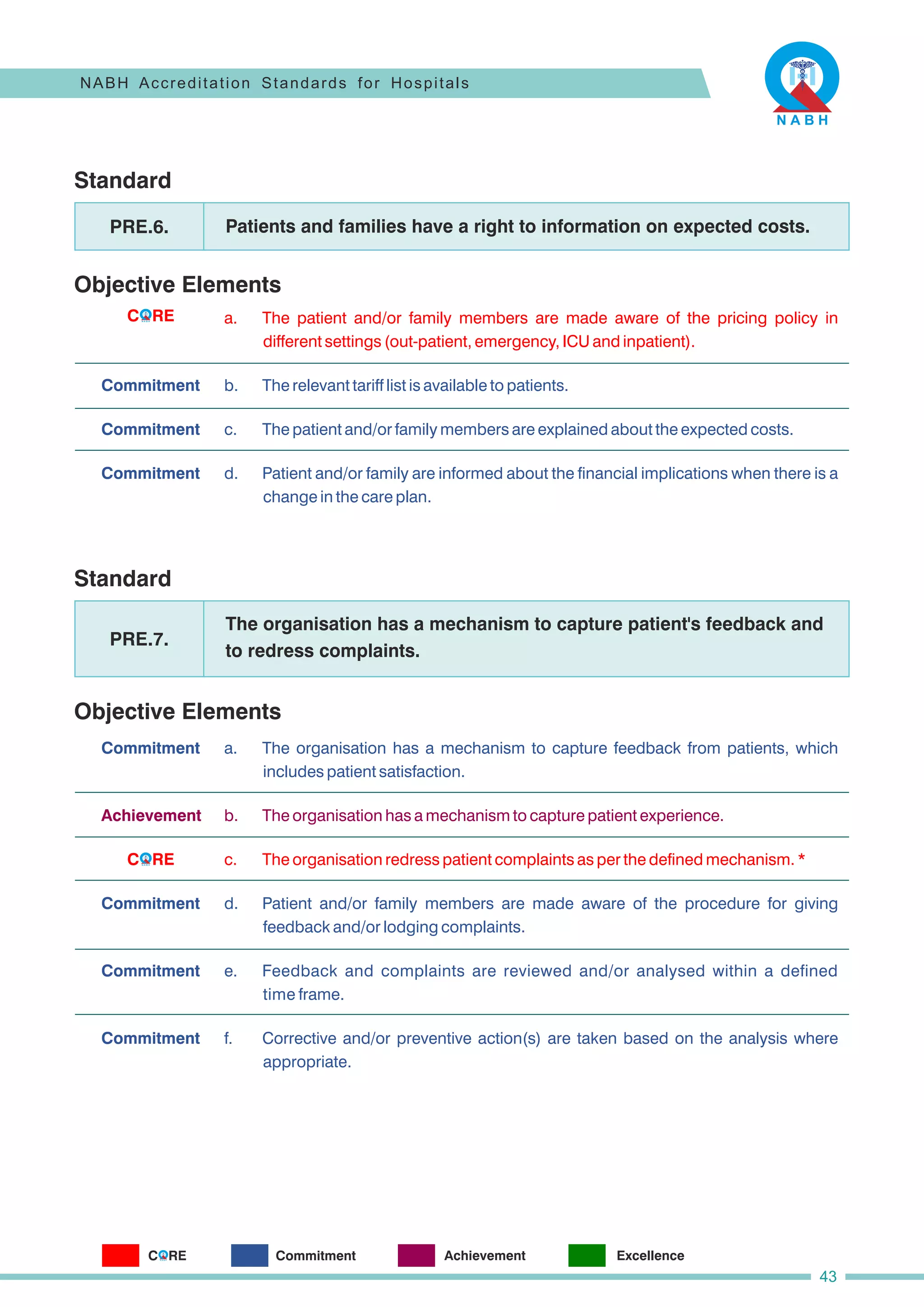
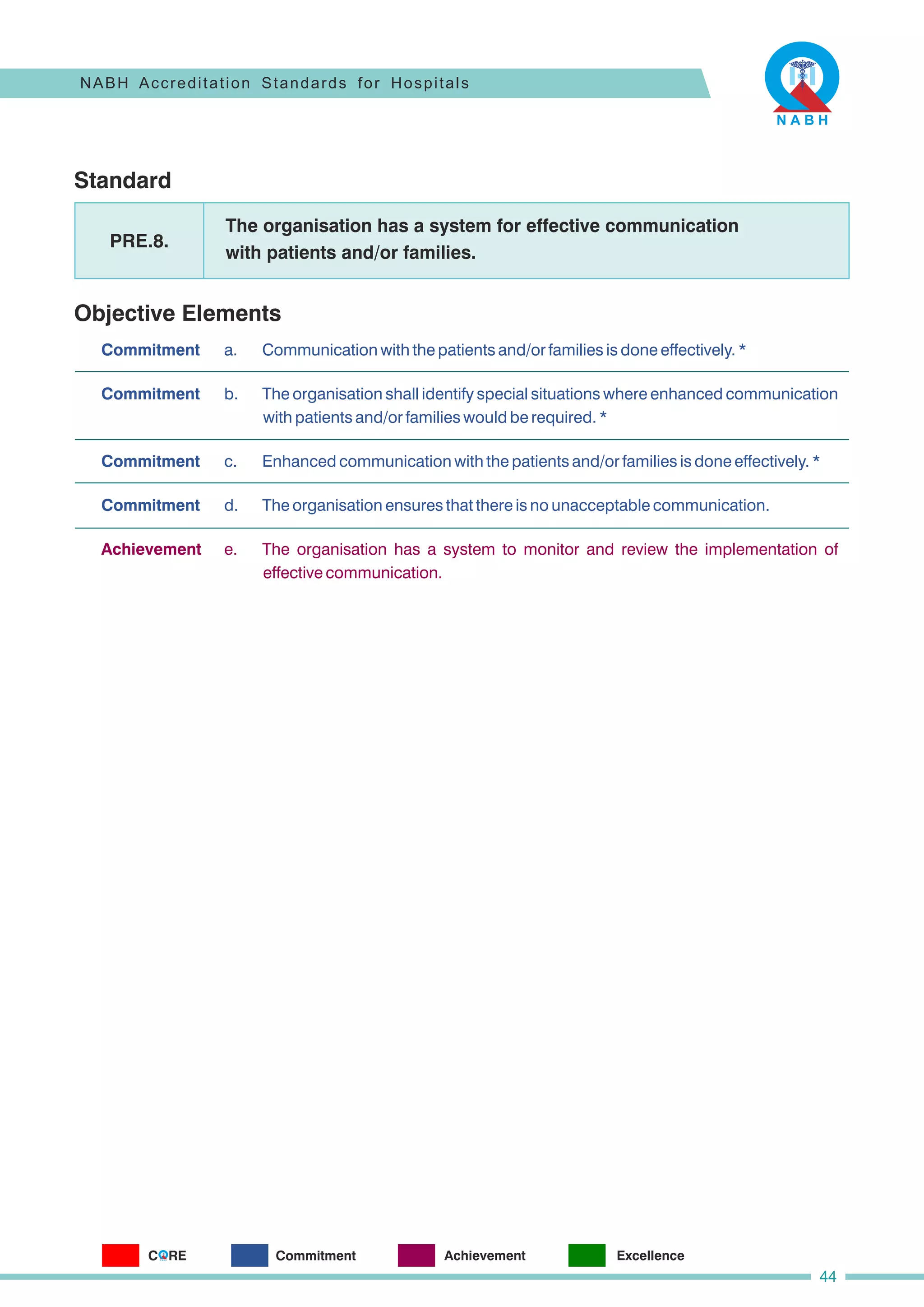
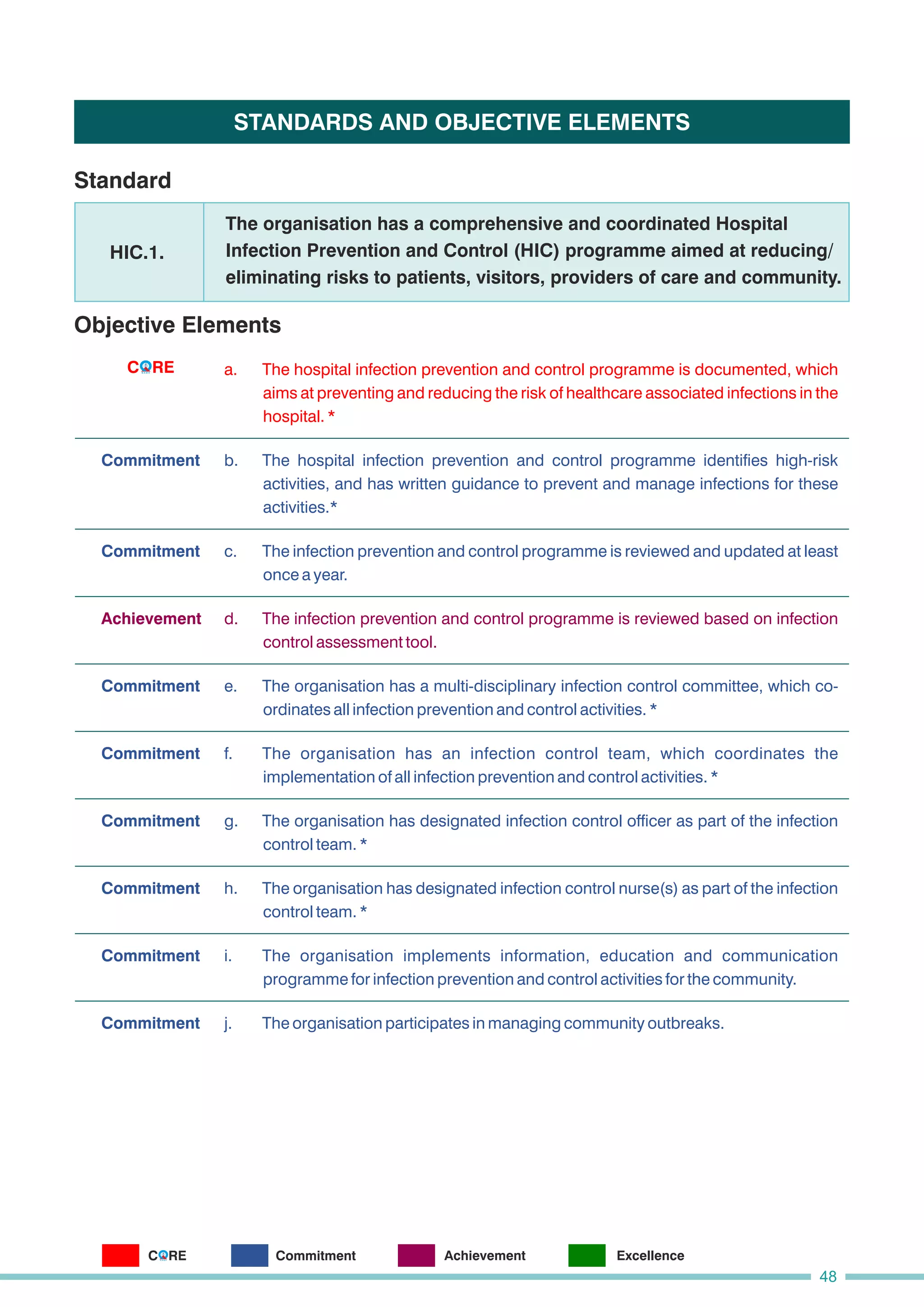
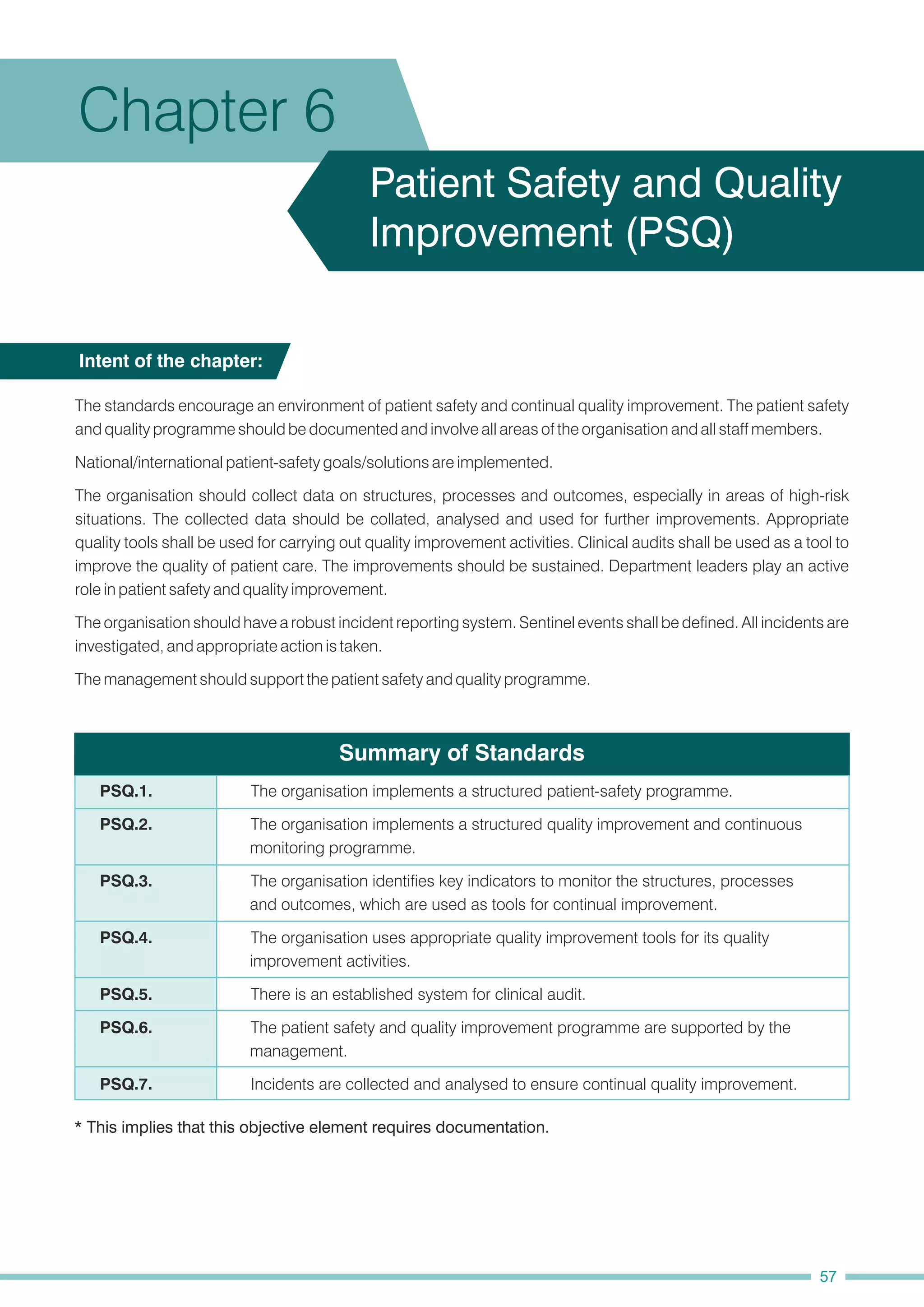
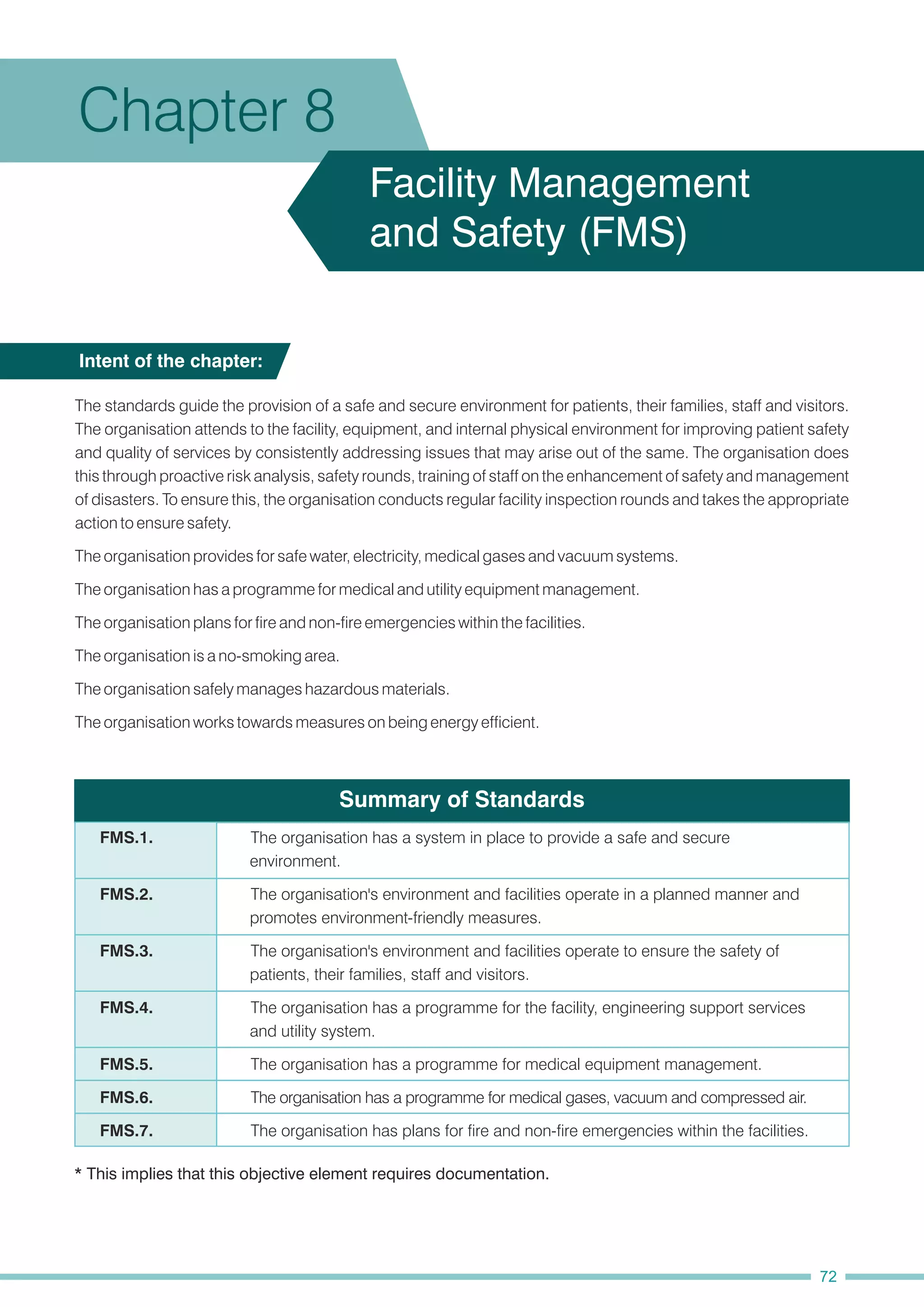
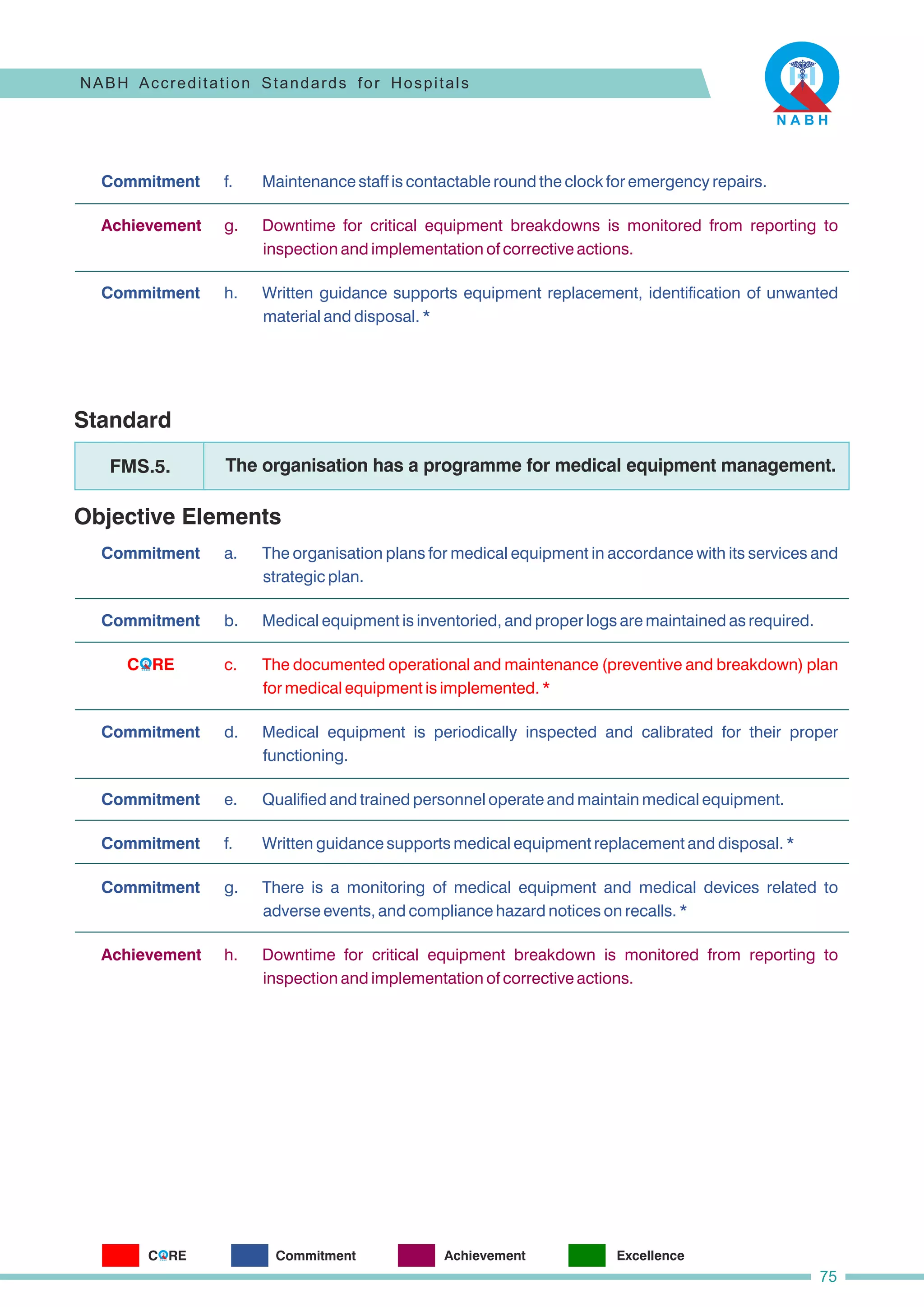
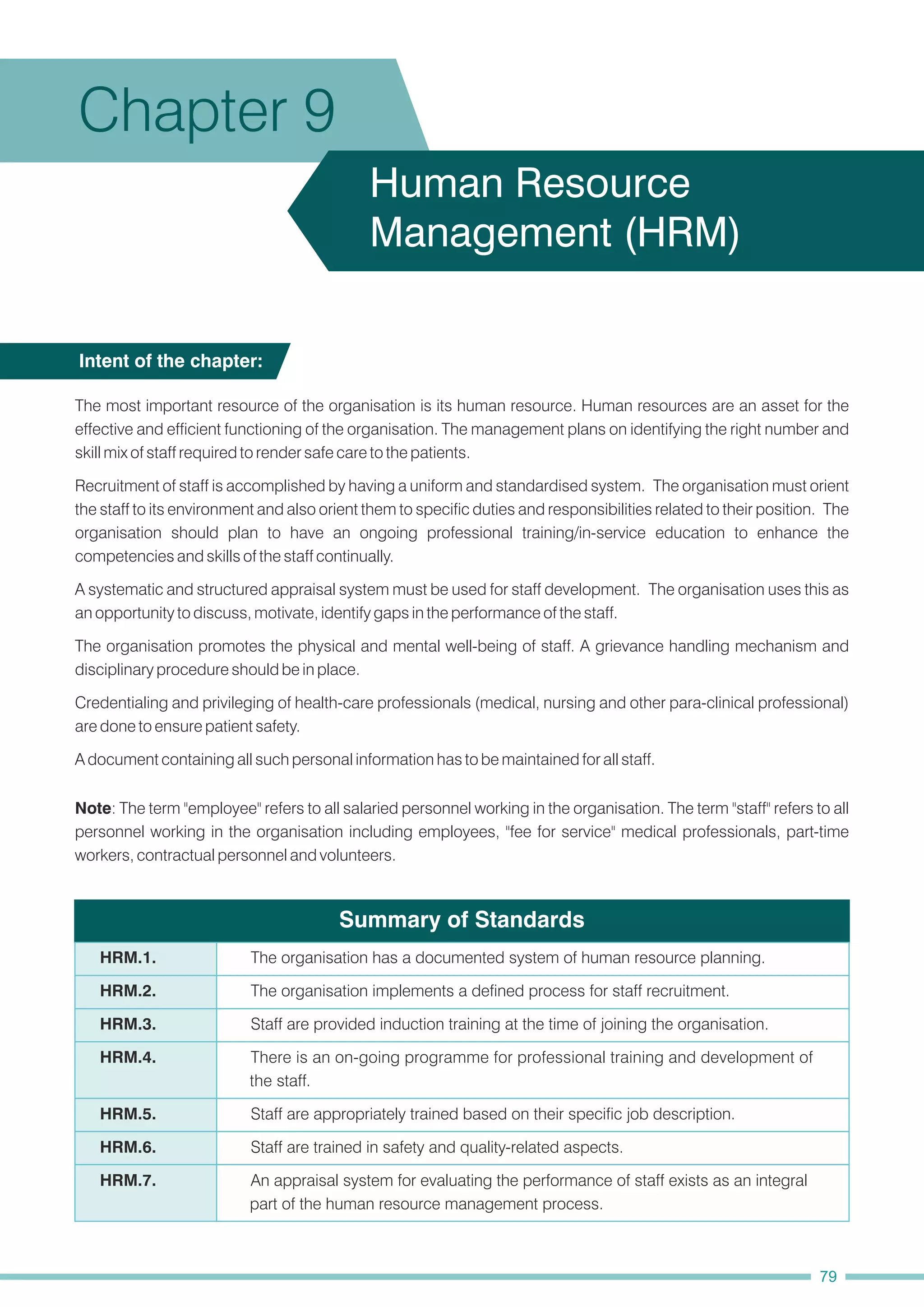
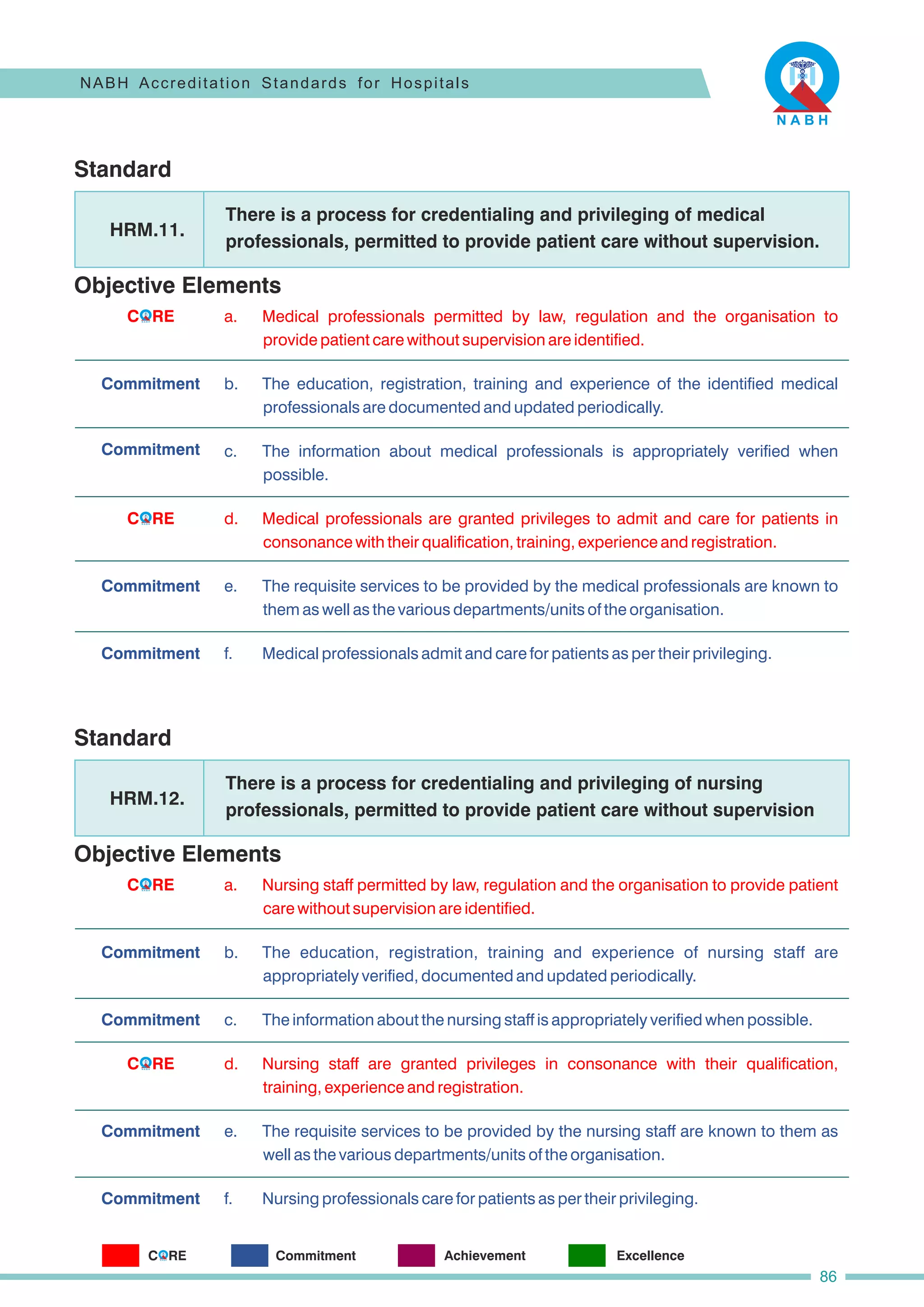
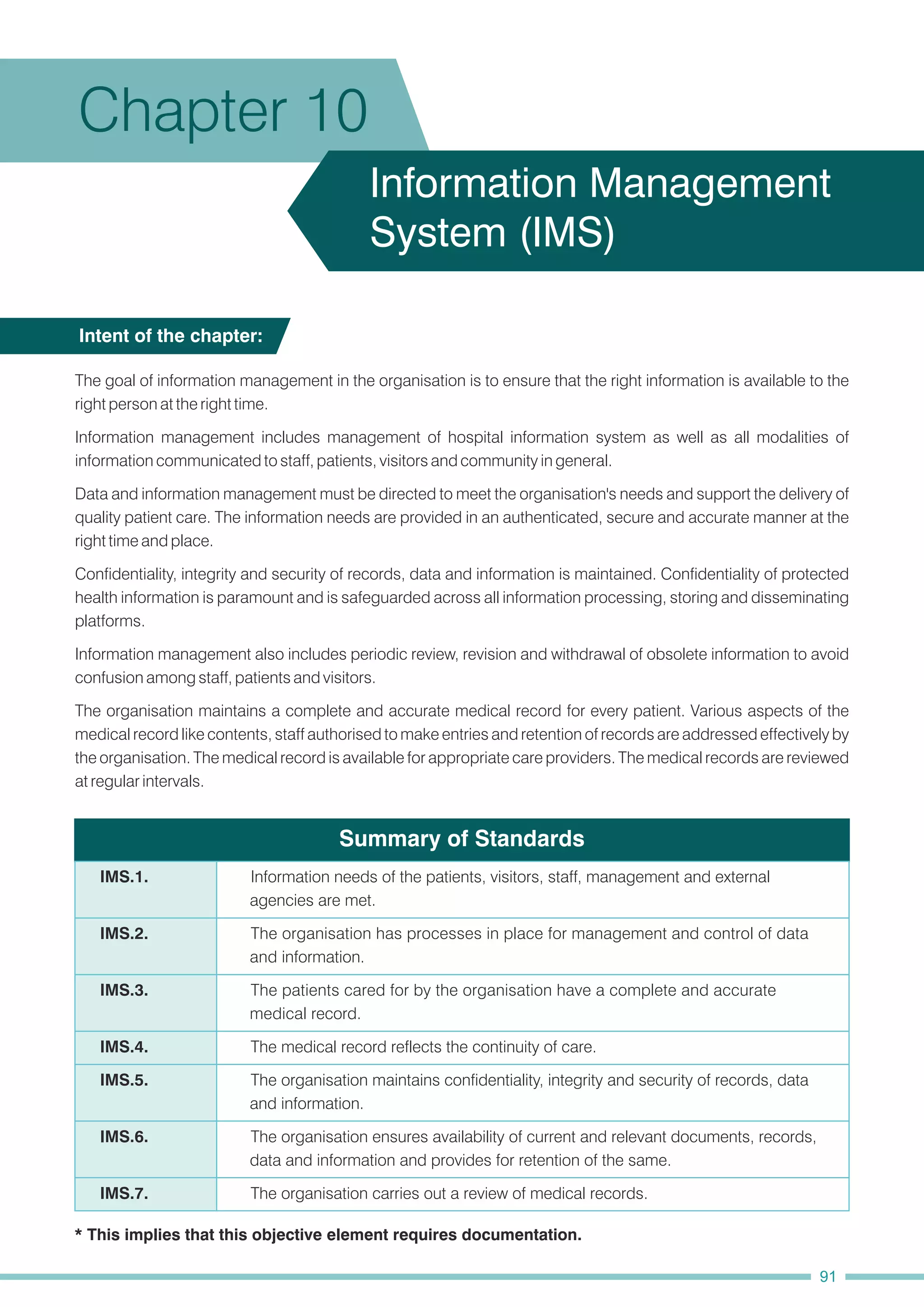
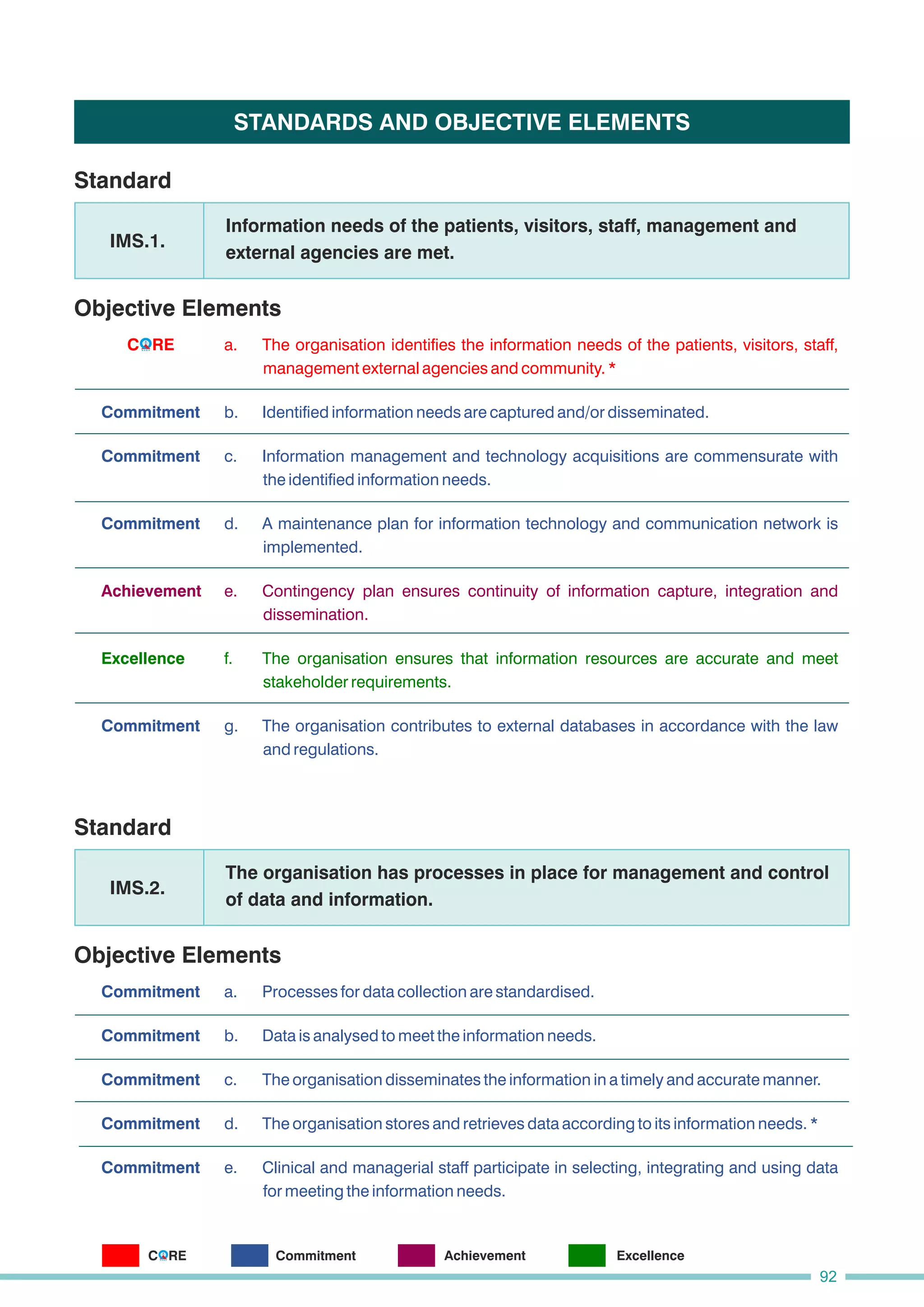
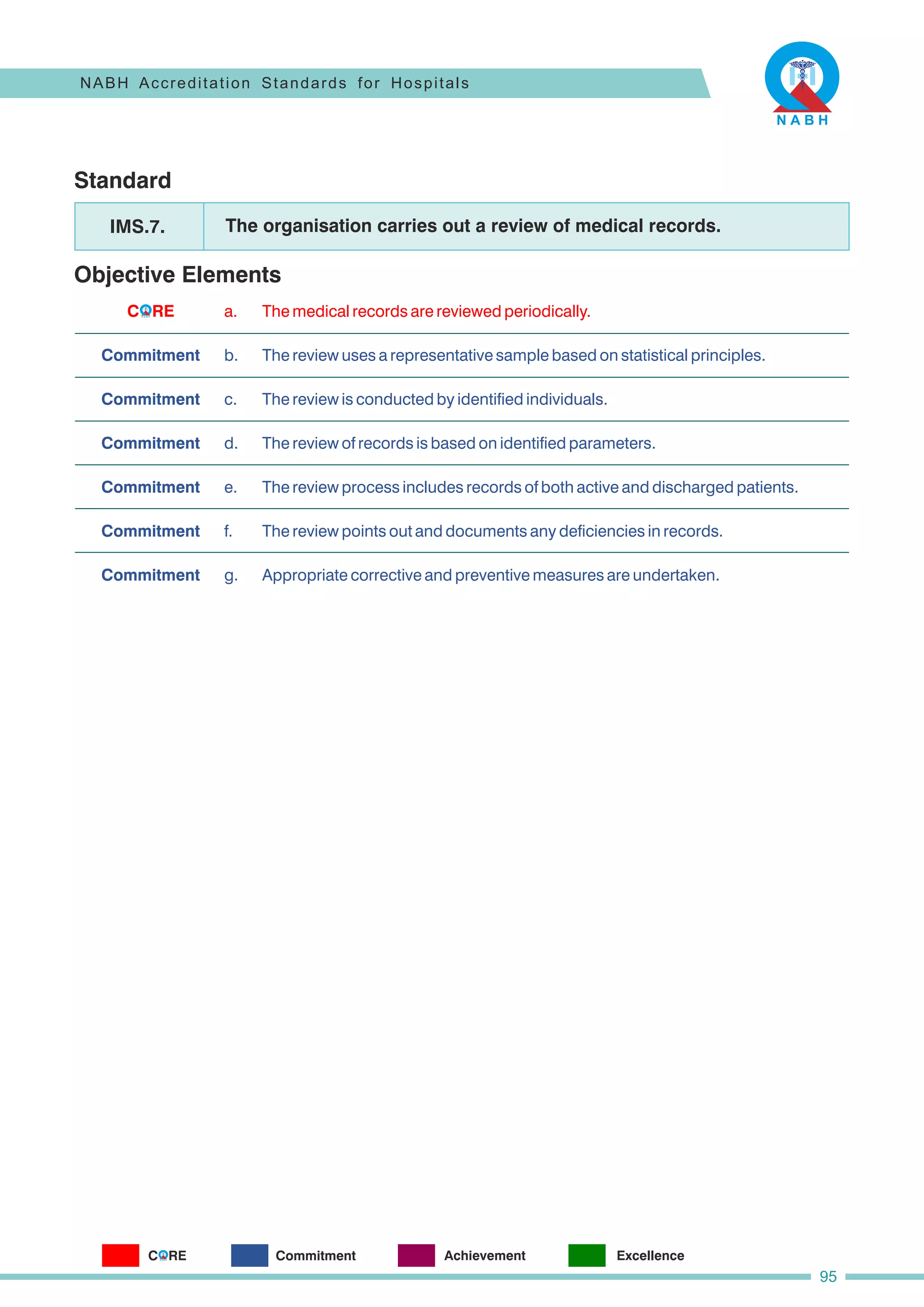
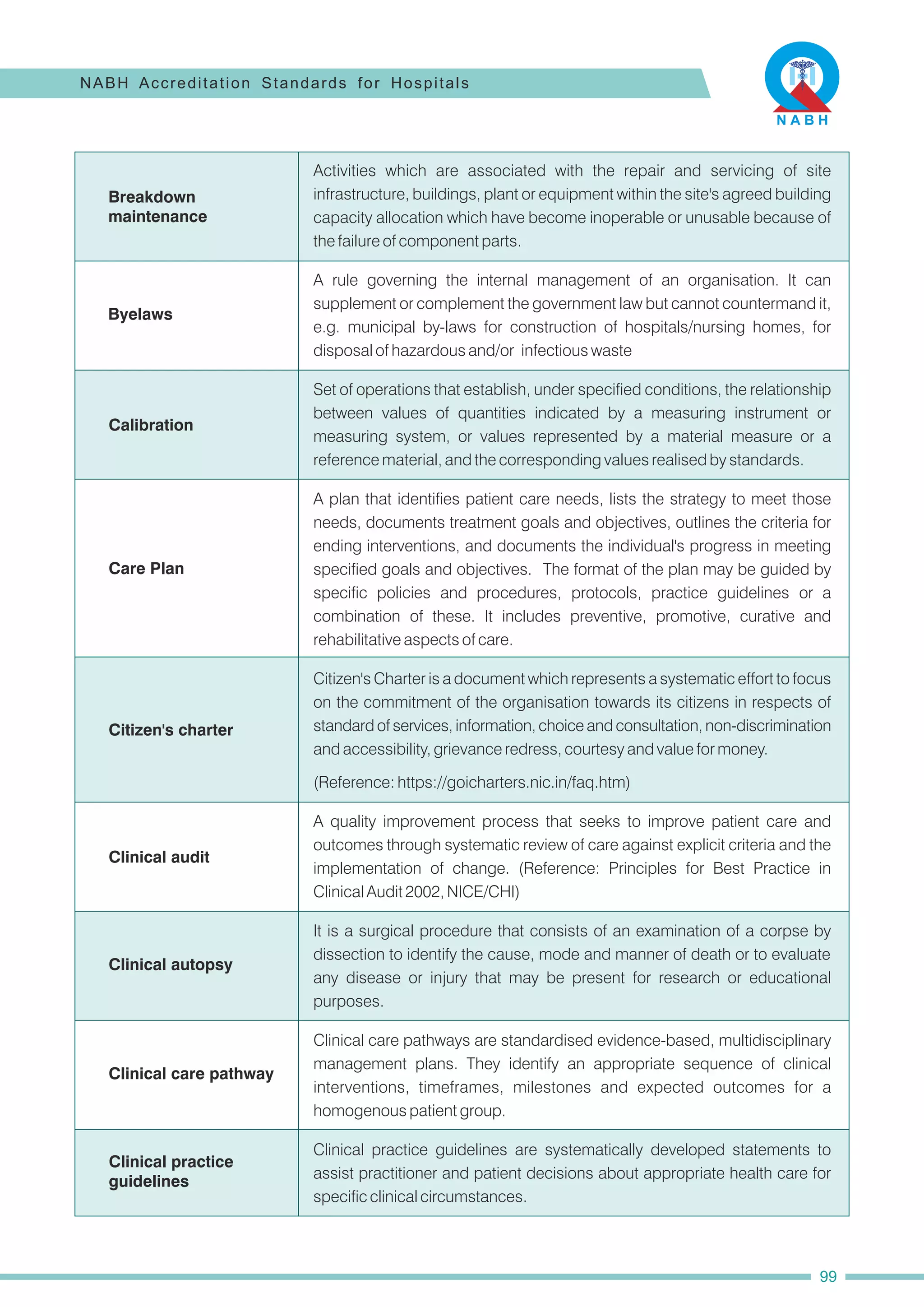
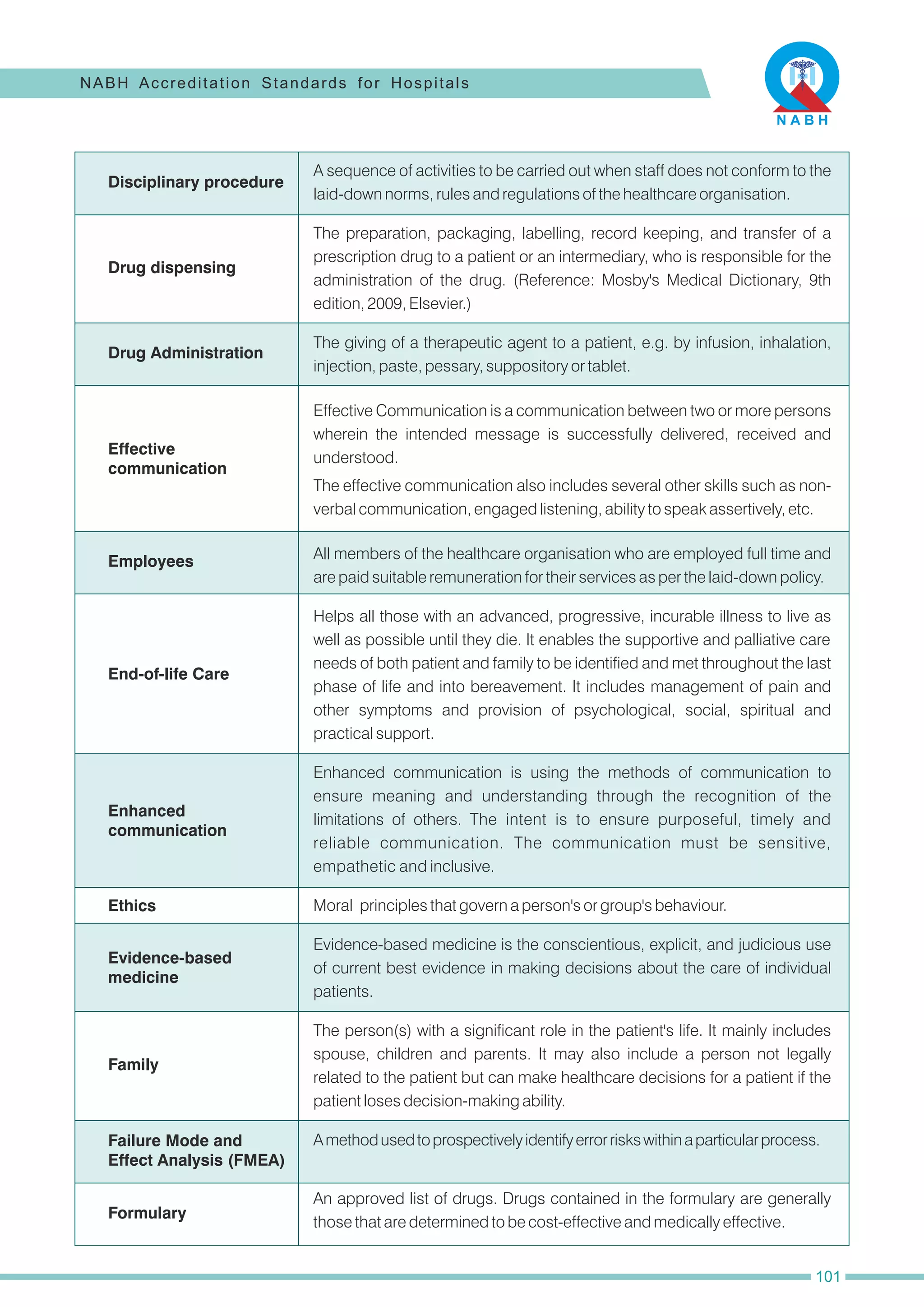
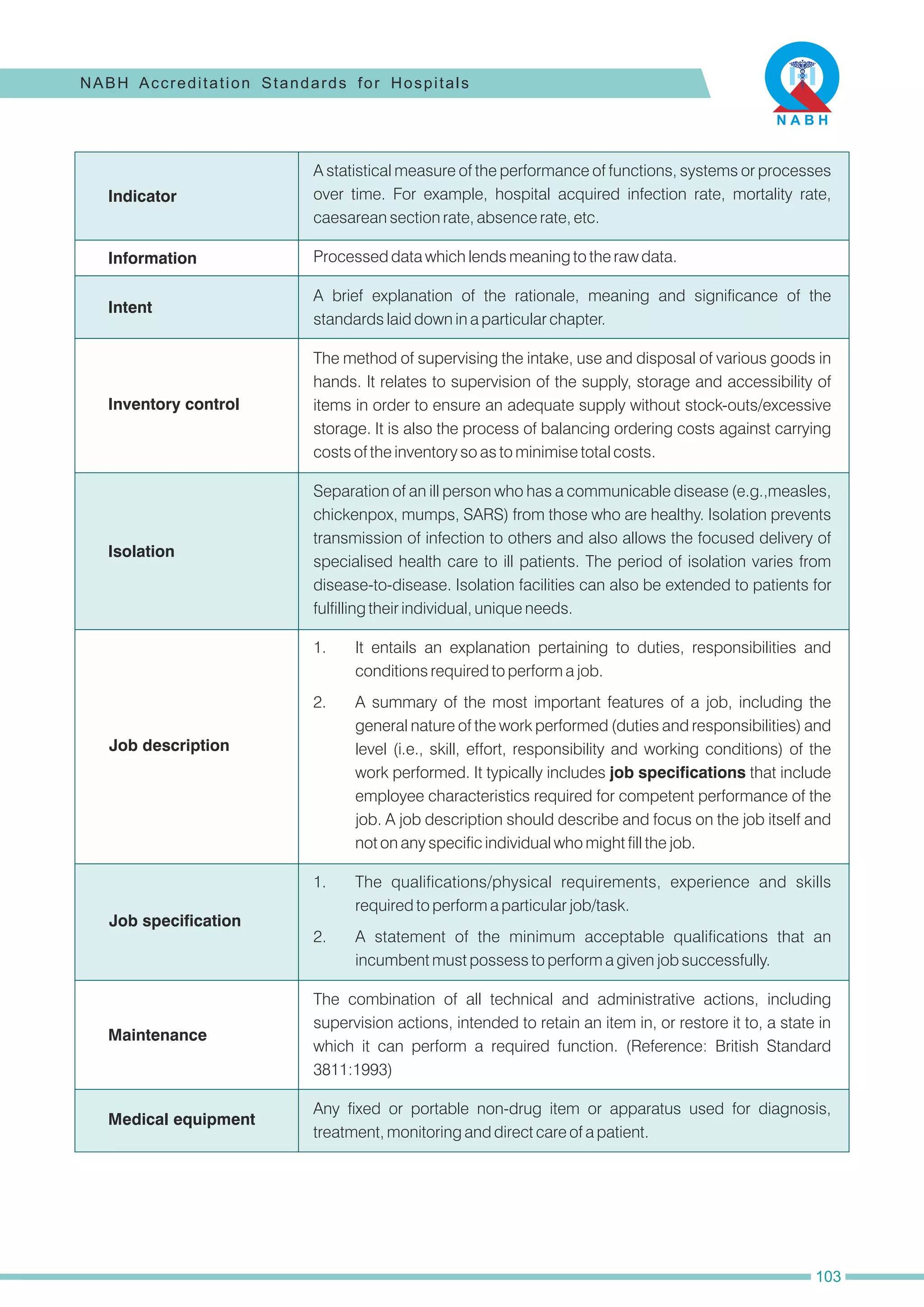
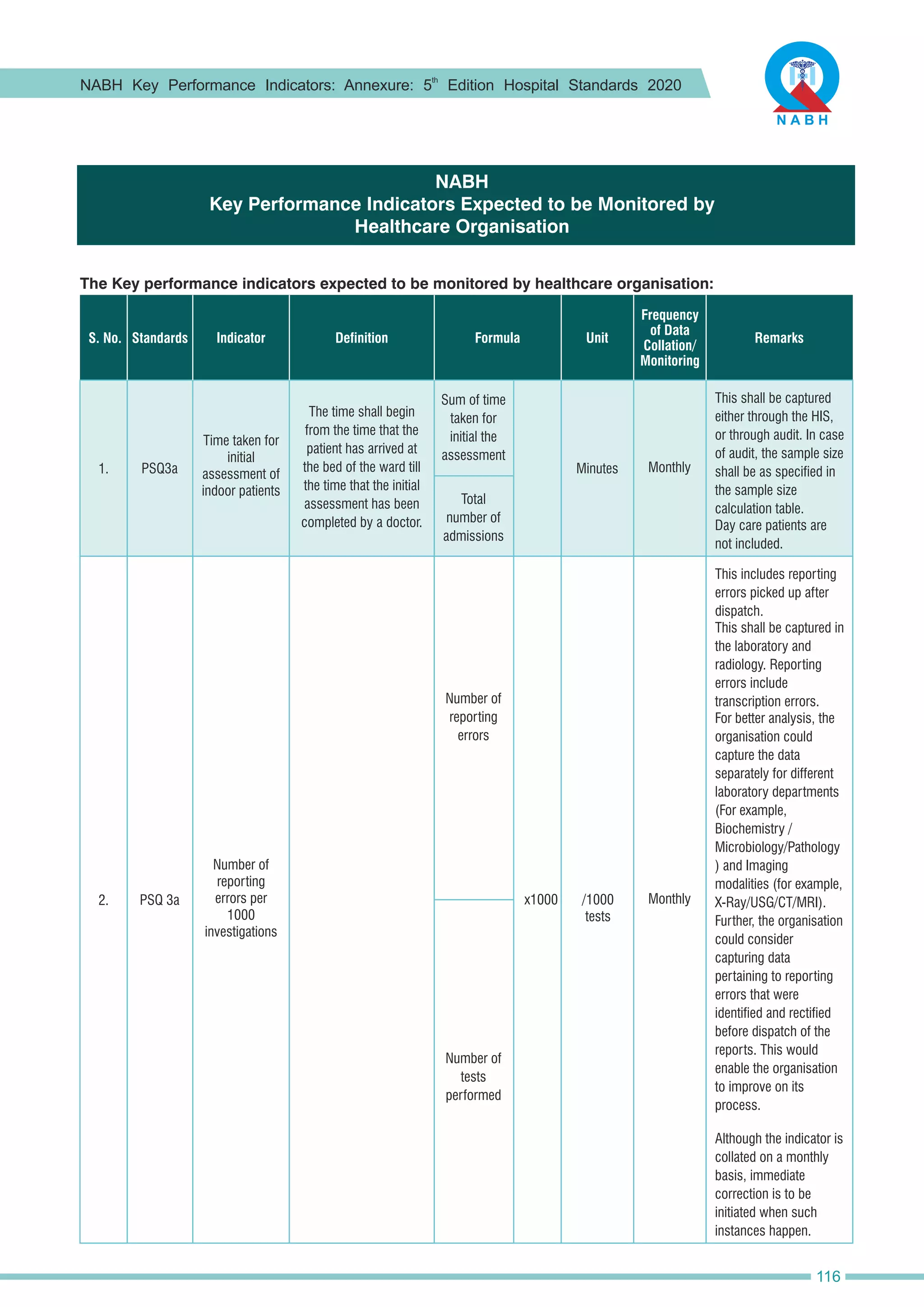
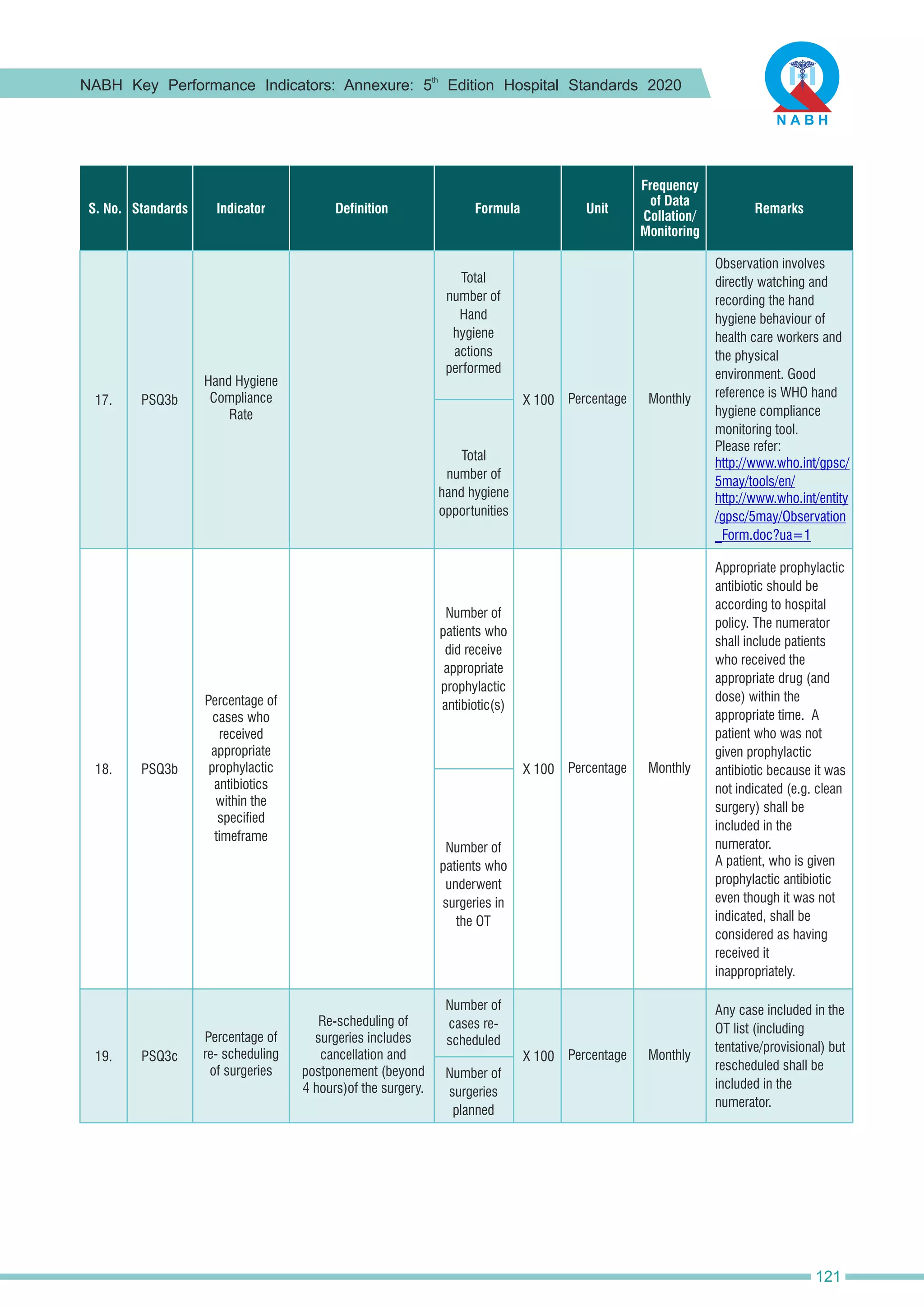
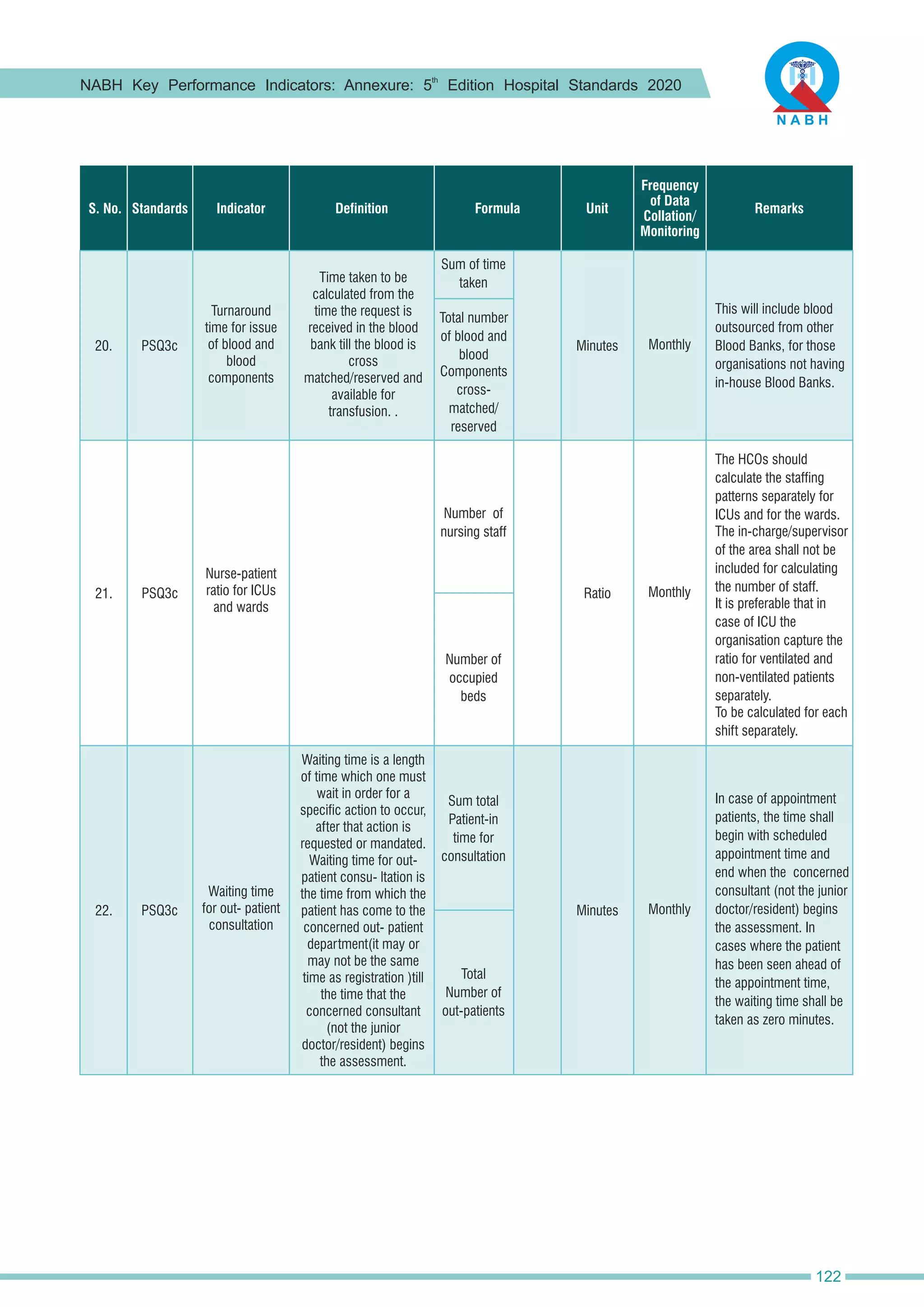
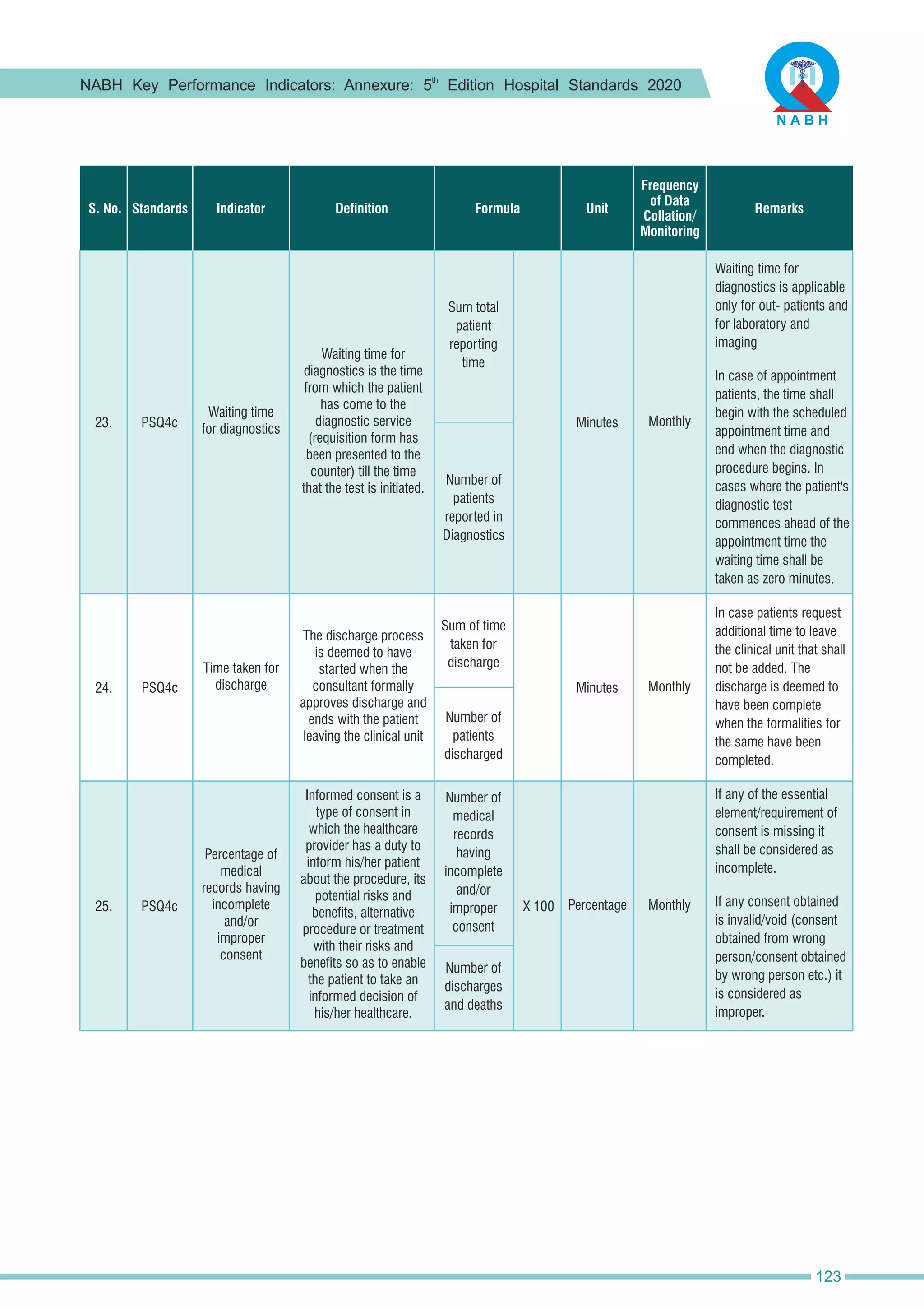
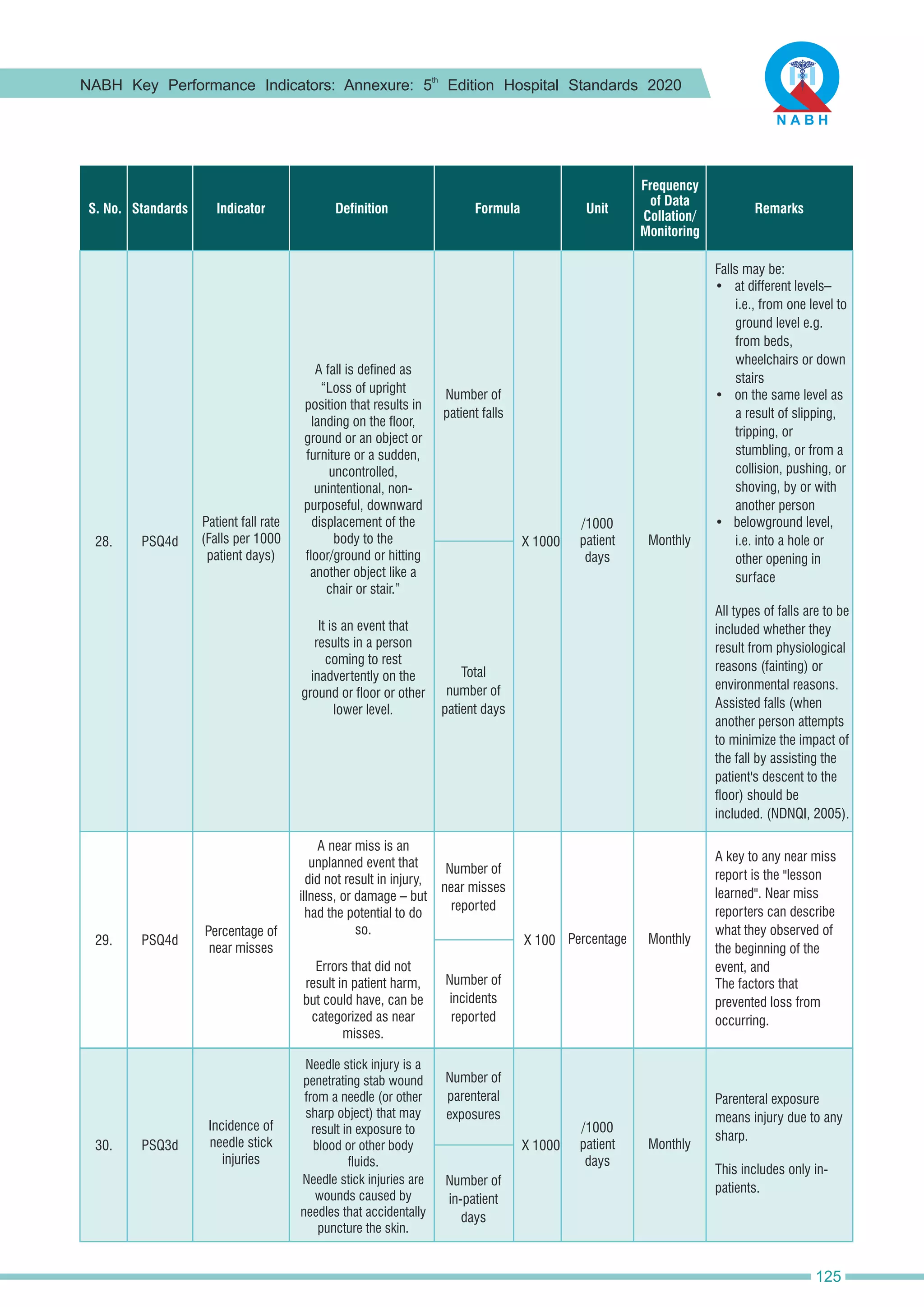
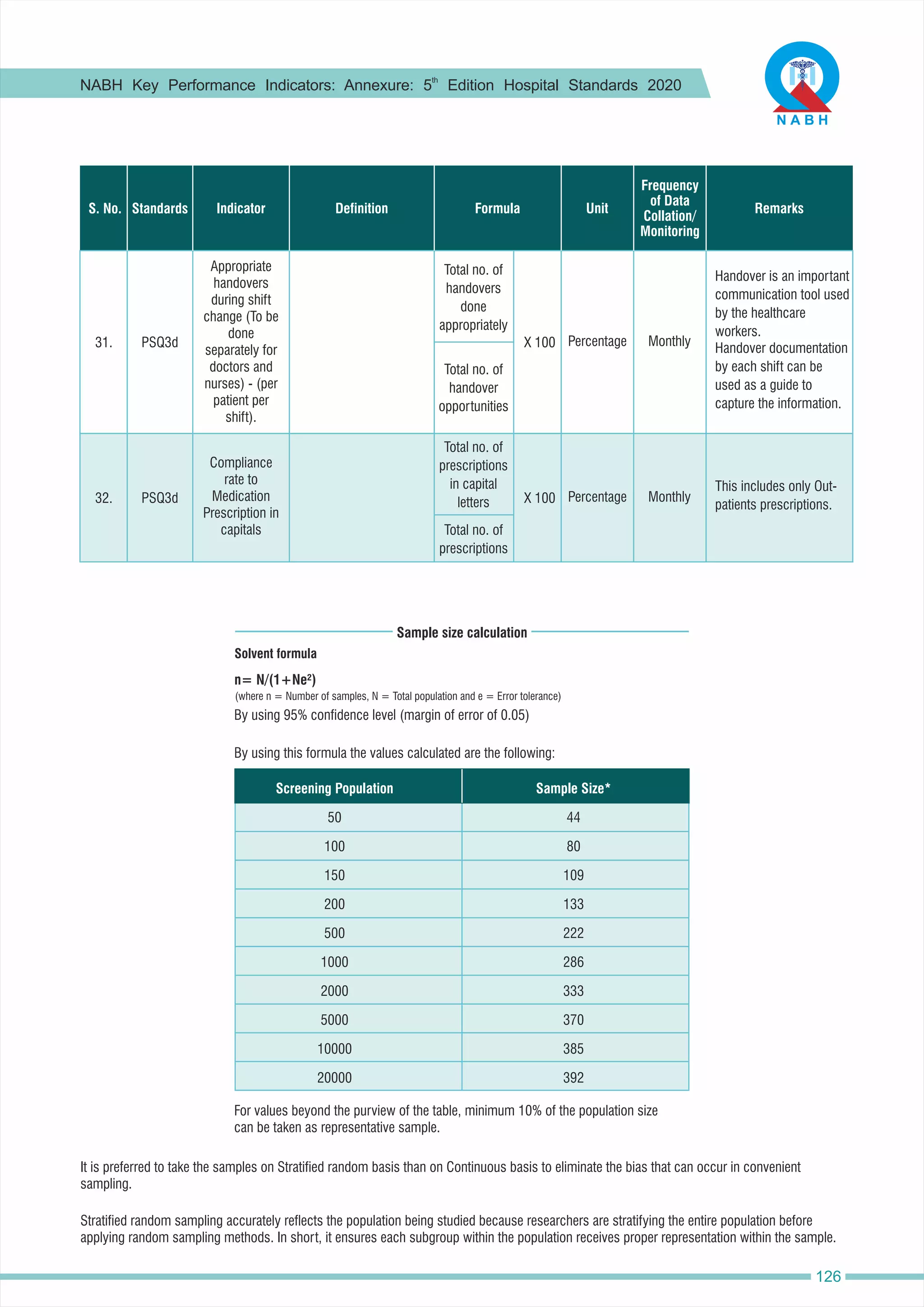
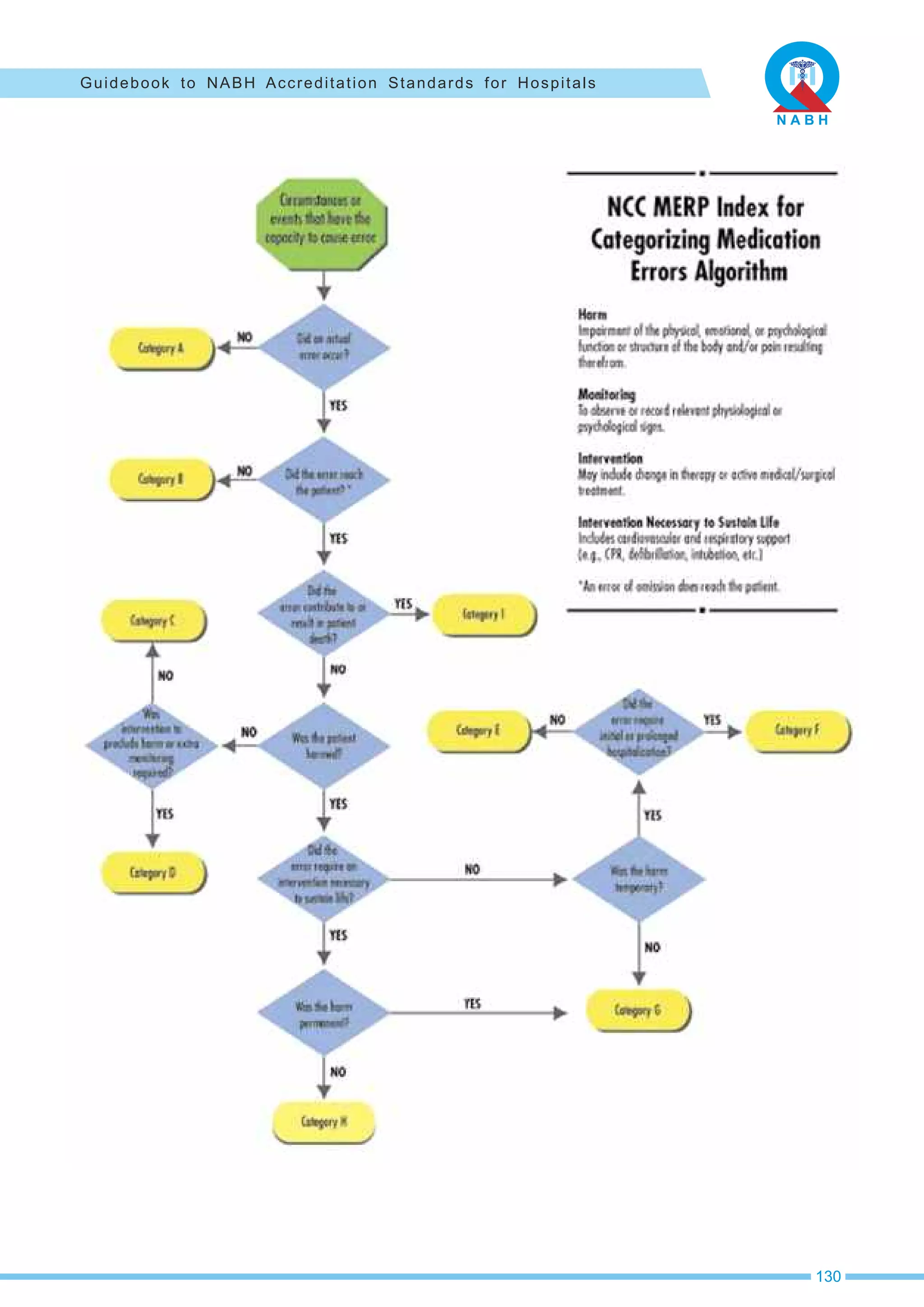
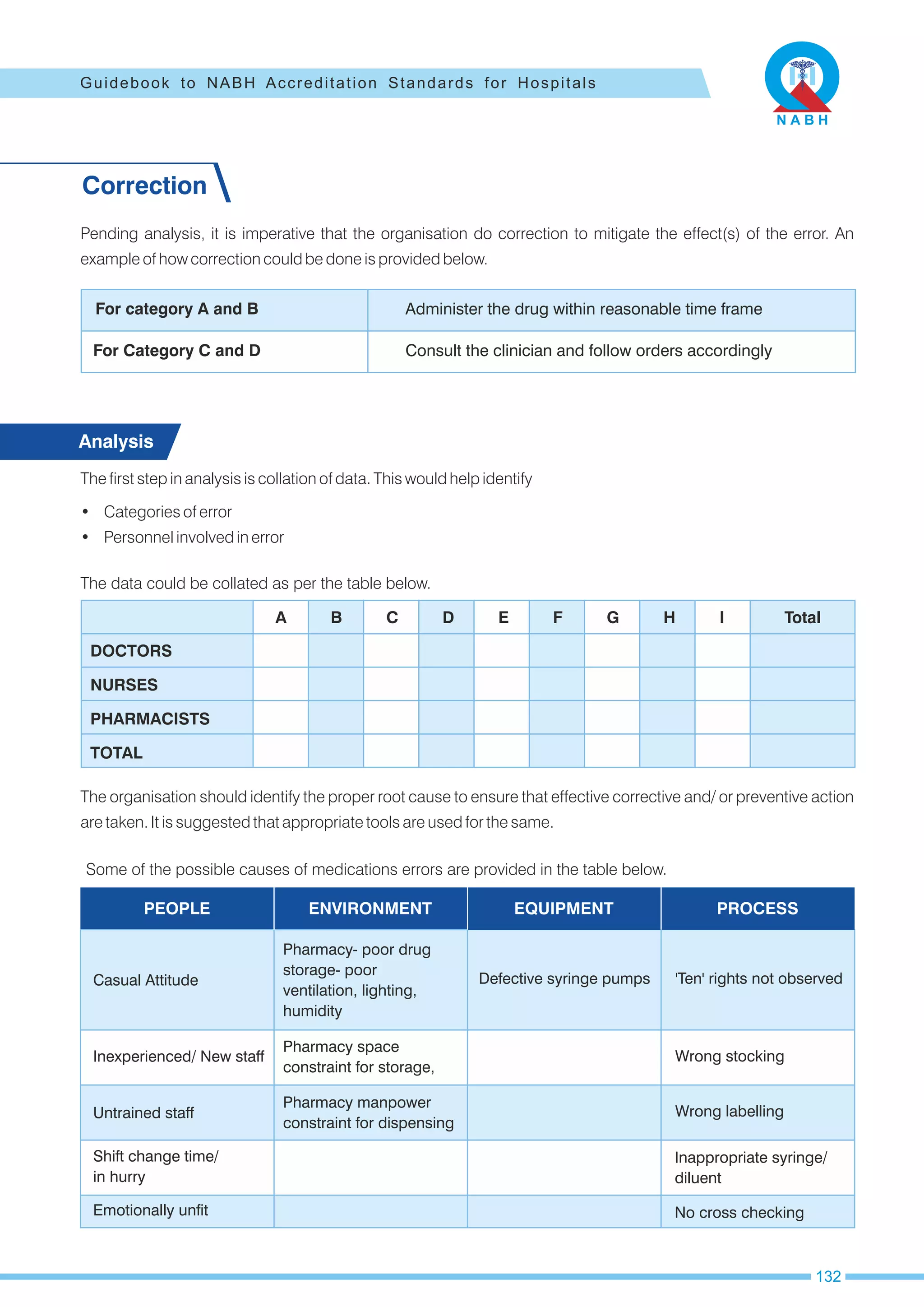
The NABH Accreditation Standards for Hospitals, 5th edition, released in April 2020, aim to enhance patient safety and quality of service delivery in healthcare institutions in India. The standards consist of 651 objective elements categorized into core, commitment, achievement, and excellence, facilitating a structured approach to quality improvement through a newly modified graded scoring methodology. The document emphasizes the importance of continuous quality improvement and fosters a supportive framework for healthcare organizations to ensure patient safety and effective service delivery.