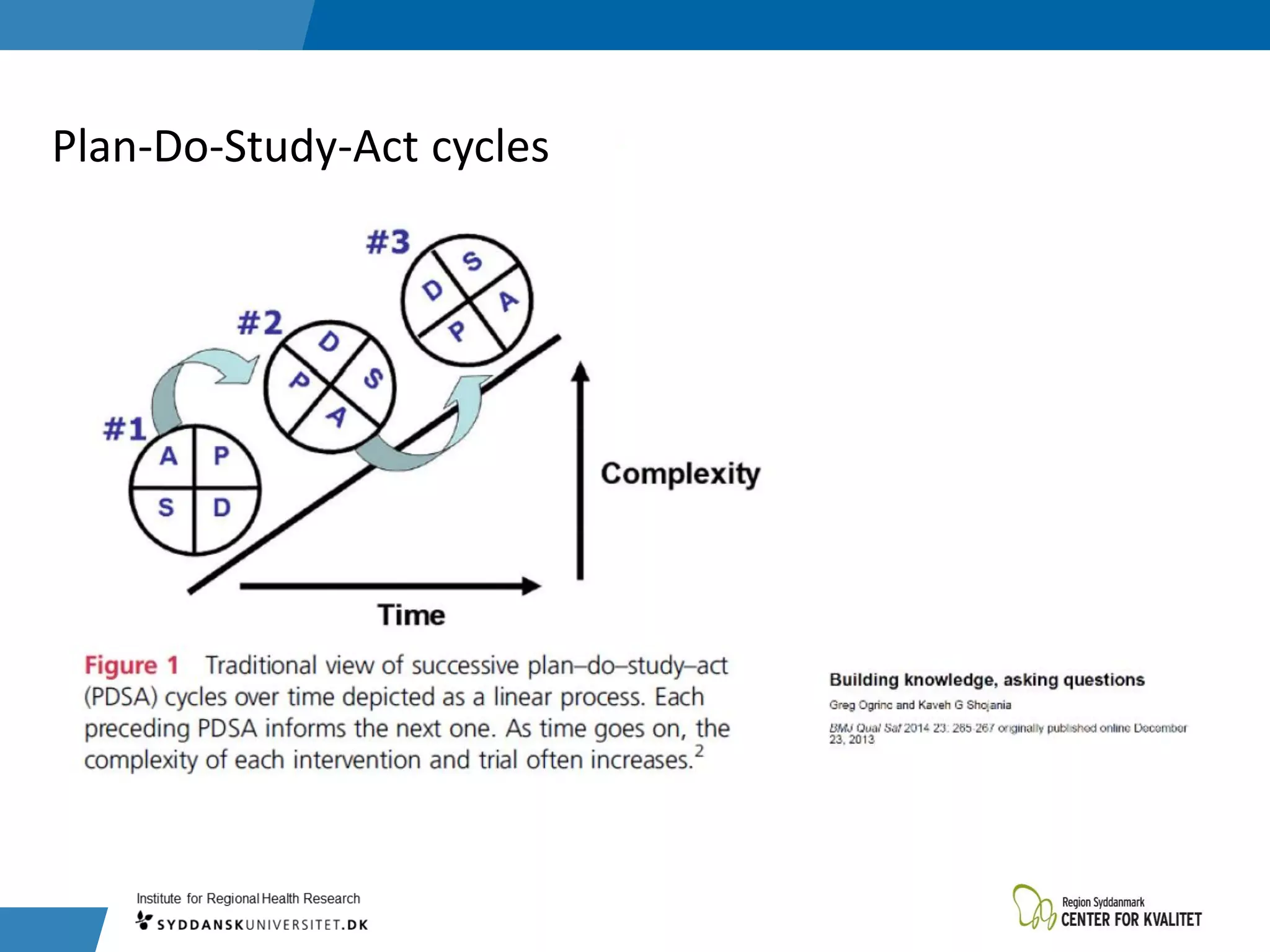
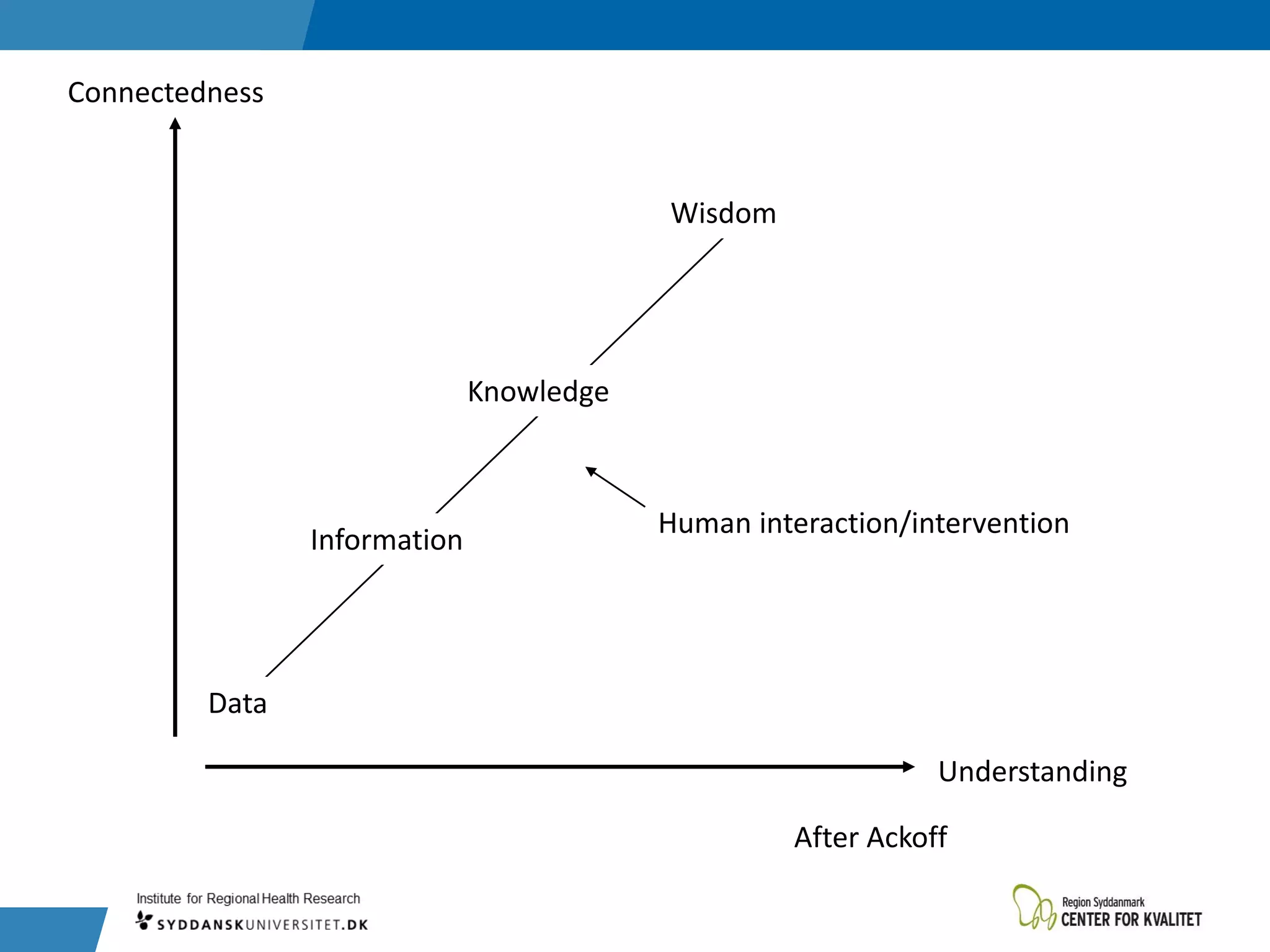
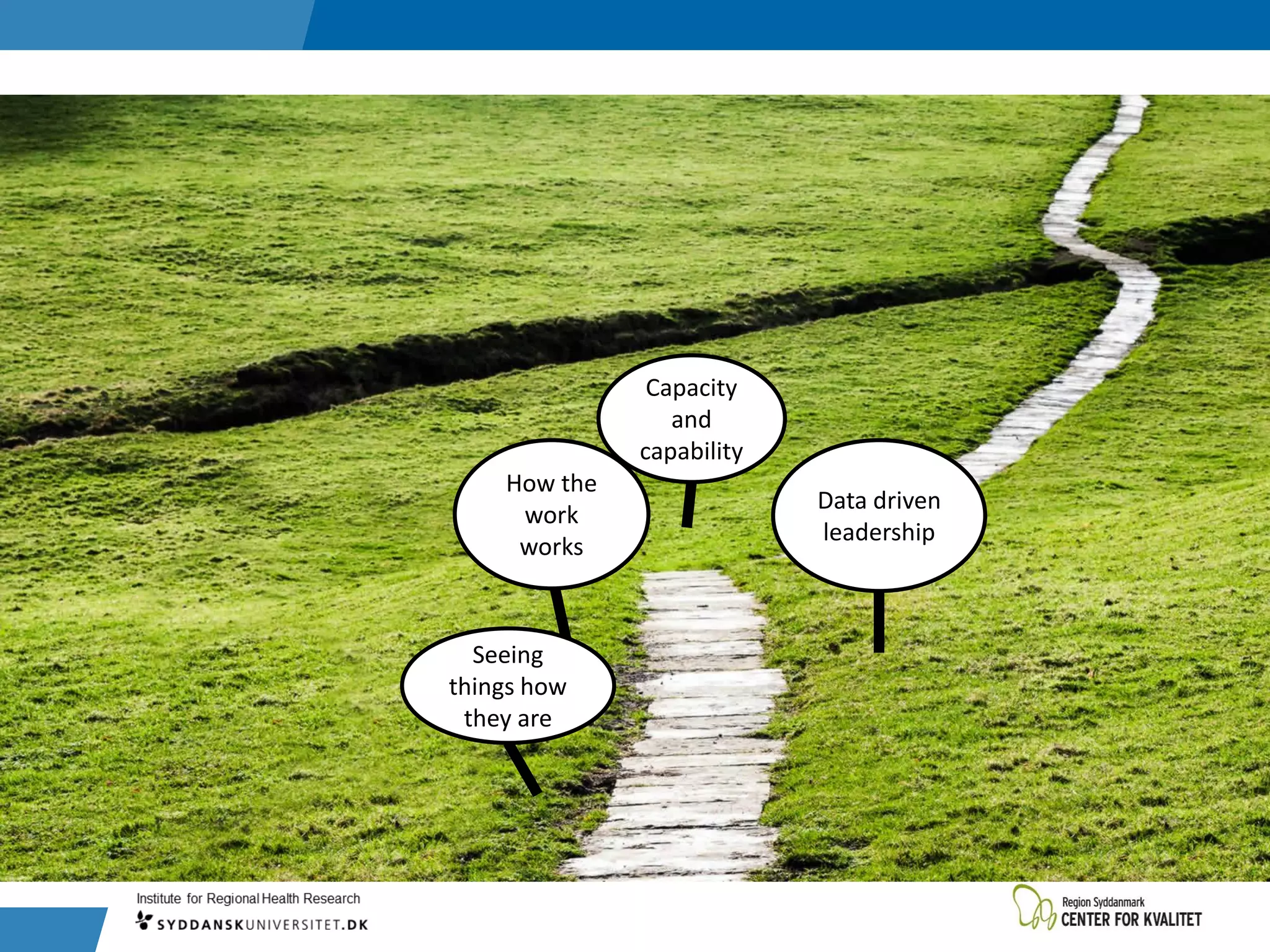
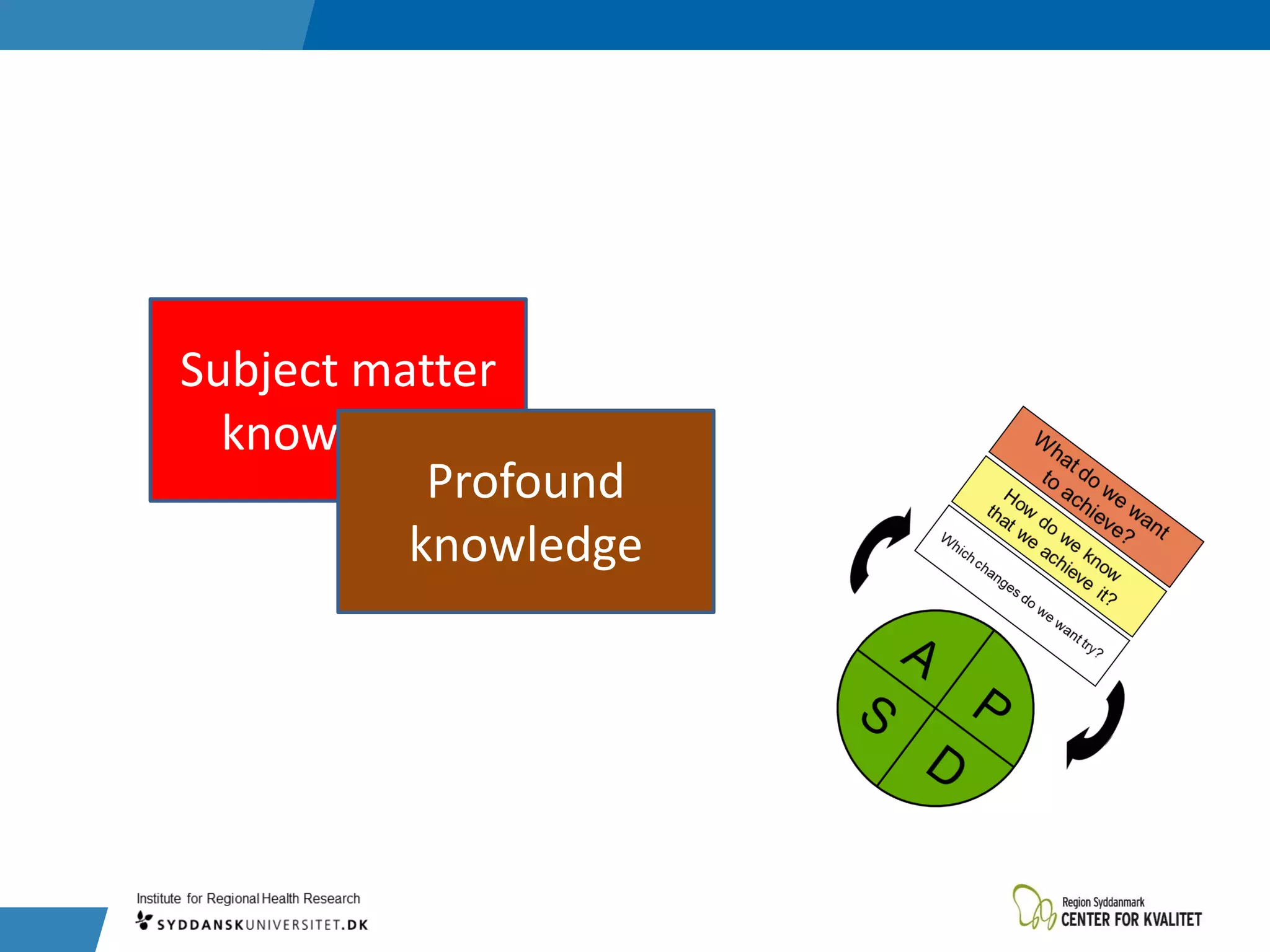
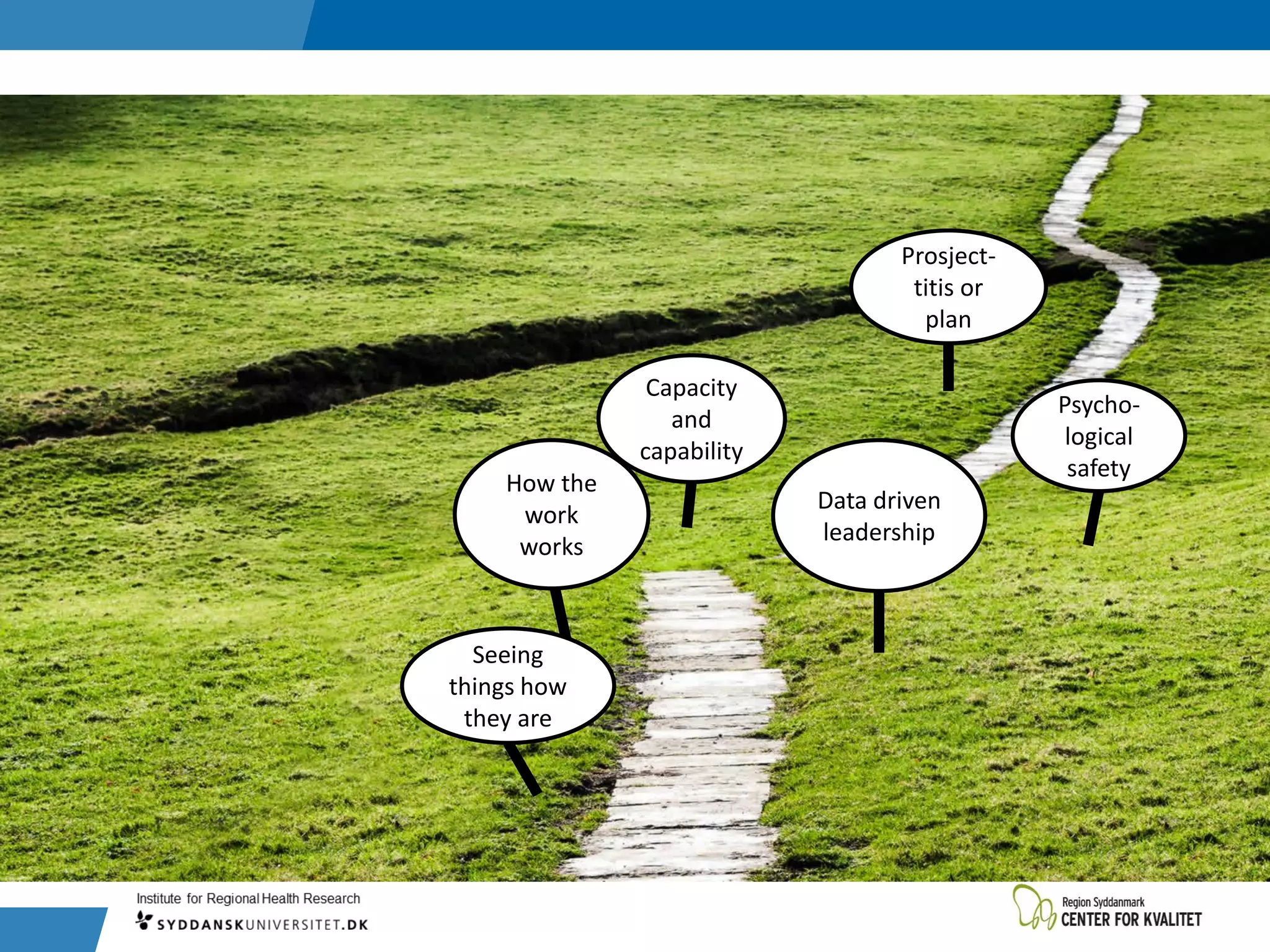
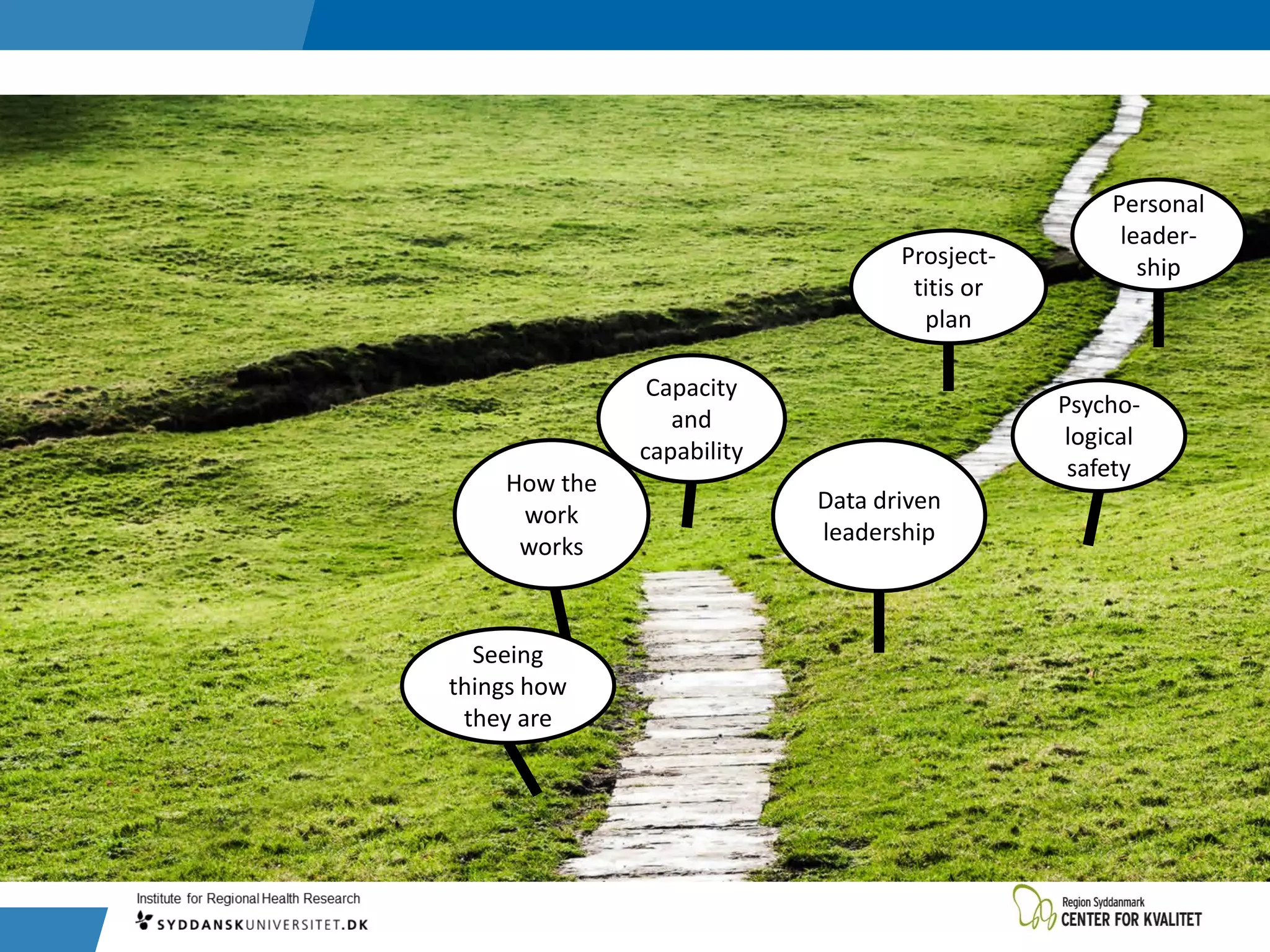
This document discusses seven key aspects of managing healthcare quality and safety: 1) seeing reality objectively, 2) understanding how work is actually performed, 3) using data to drive leadership decisions, 4) developing organizational capacity and individual capabilities, 5) cultivating psychological safety, 6) avoiding too many improvement projects, and 7) the importance of personal leadership. It provides references and insights from experts in the field on each of these topics to support healthcare quality improvement efforts.






























![”I would rather have my ignorance than
another men’s knowledge, because I have got
so much of it.”
P 250—Mark Twain’s letters [1917 ed.], Vol 1](https://image.slidesharecdn.com/20181113managementofqicple-181114152215/75/2018-11-13-management-of-qi-cple-42-2048.jpg)