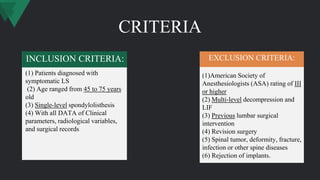
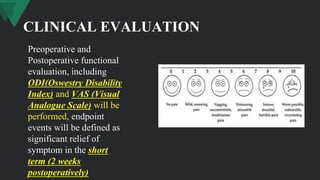
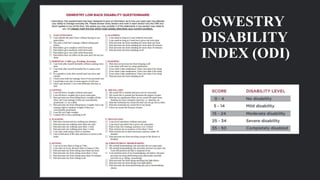
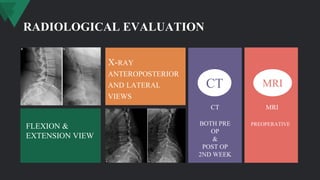
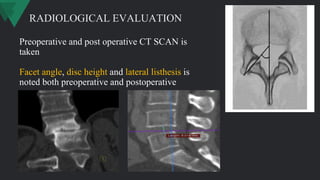
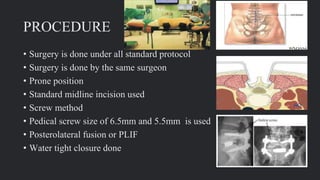
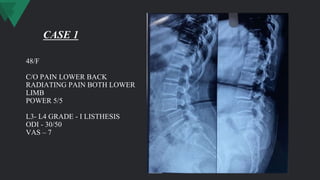
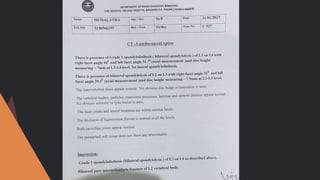
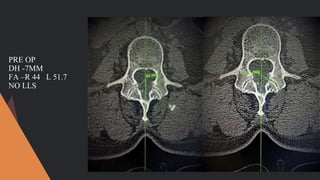
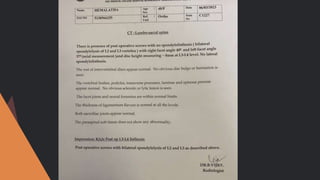
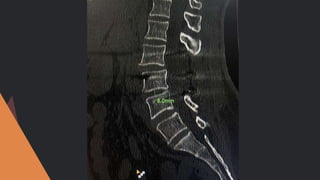
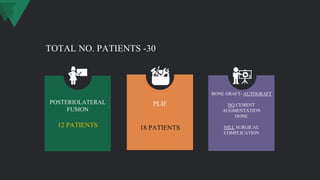
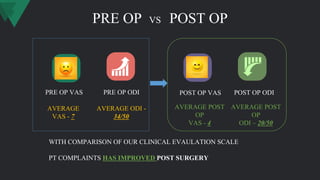
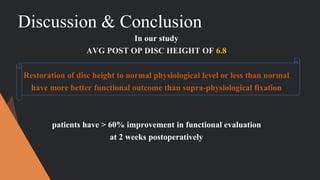
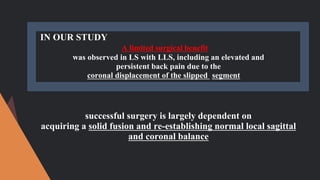
This study evaluates predictors of unfavorable clinical outcomes in patients with lumbar spondylolisthesis after fusion. Conducted on 30 patients, it concludes that restoring disc height to normal levels and addressing lateral slippage are crucial for better functional recovery, with significant improvements noted in Oswestry Disability Index (ODI) and Visual Analog Scale (VAS) scores post-surgery. The results suggest that surgical success is dependent on achieving solid fusion and restoring sagittal balance.