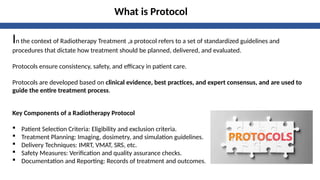
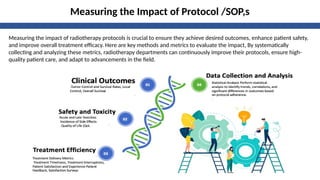
The document discusses the development, implementation, and evaluation of protocols in radiotherapy treatment to enhance consistency, safety, and effectiveness. It outlines the importance of standardized procedures, the roles of multidisciplinary teams, and the necessity of regular updates to adapt to advancements in the field. Continuous evaluation of these protocols is crucial for improving patient outcomes and ensuring high-quality care.