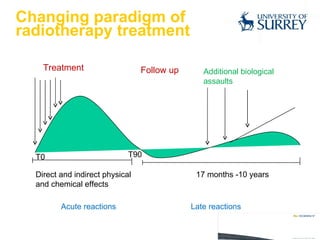
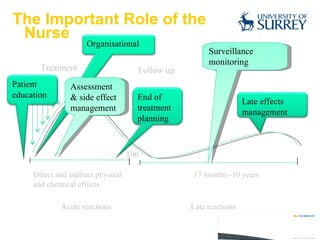
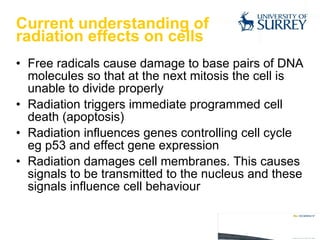
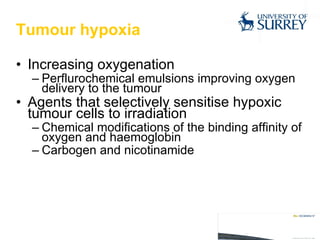
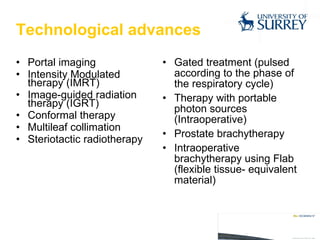
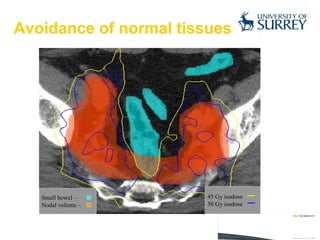
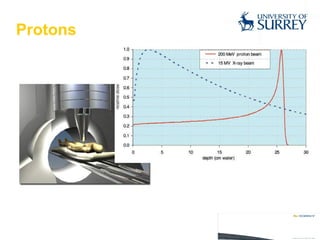
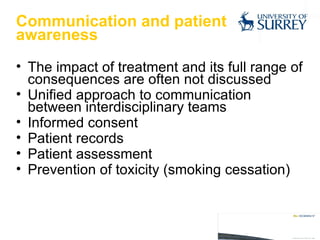
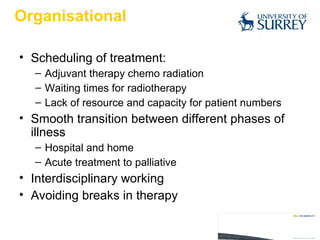
Radiotherapy is an important treatment for many cancers. There have been several developments in radiotherapy, including biological and physical optimizations, that allow for more targeted treatment with fewer side effects. Nurses play a key role in assessing patients, managing side effects, providing education and support, and coordinating care. Continued technological advances and multidisciplinary care seek to further improve radiotherapy outcomes.