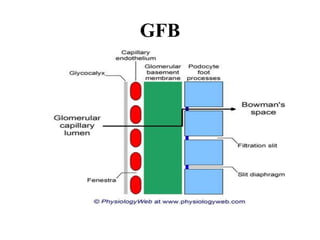
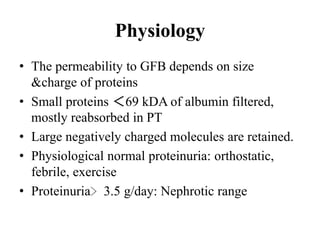
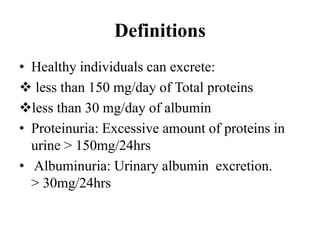
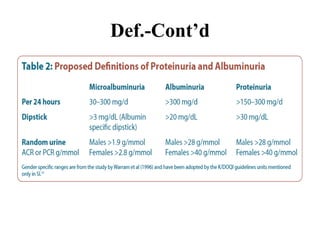
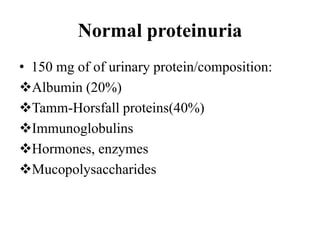
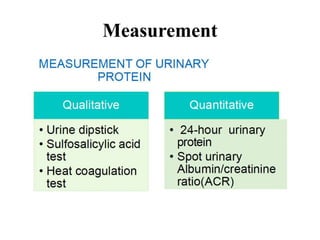
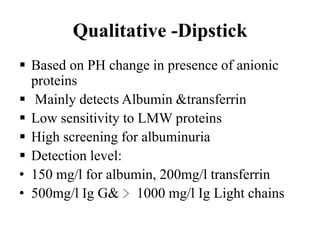
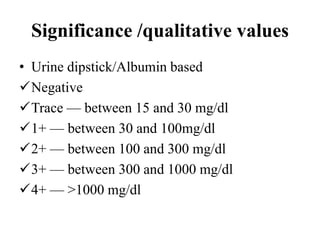
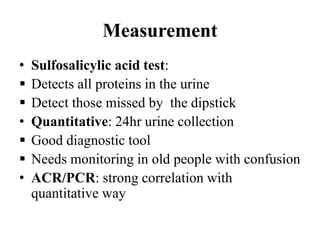
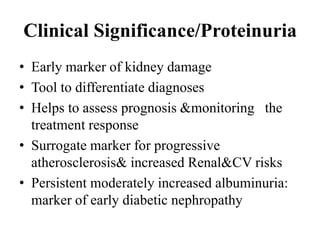
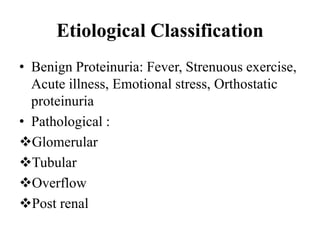
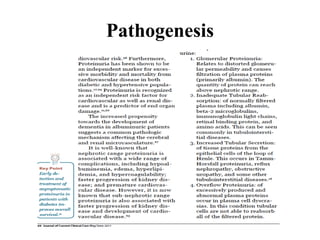
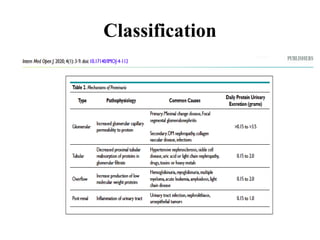
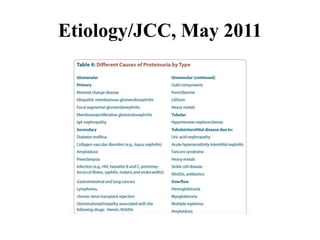
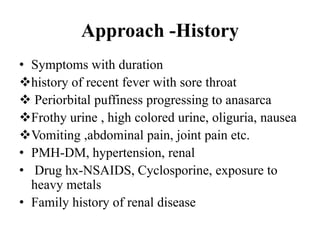
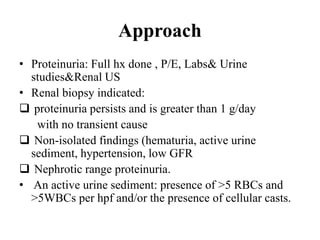
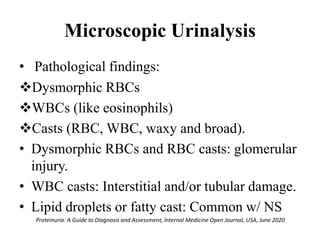
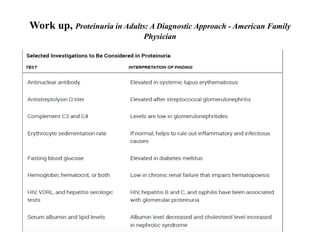
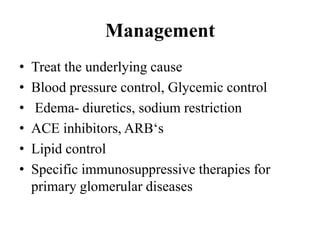
Dr. Prosper's presentation covered the approach to proteinuria. It began with background on proteinuria and the basic physiology of the glomerular filtration barrier (GFB). Proteinuria was defined as excessive proteins in urine over 150mg/24hrs. Measurement methods including dipstick tests and 24hr urine collections were discussed. The etiology of proteinuria was classified as benign, glomerular, tubular, overflow or post renal. A thorough history, physical exam, labs, urine studies and renal ultrasound were recommended in the evaluation. A renal biopsy may be indicated in persistent cases. Treatment focuses on controlling underlying causes like diabetes or hypertension and reducing cardiovascular risk factors.