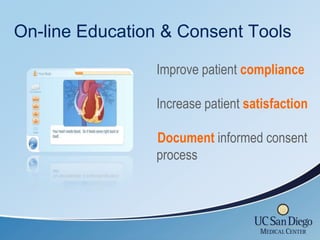
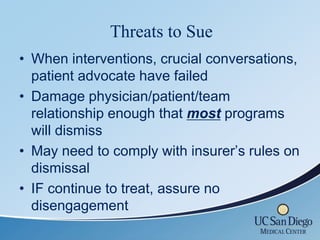
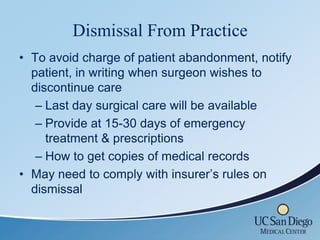
This document provides tips for managing the risk of lawsuits related to bariatric surgery practices. It discusses the importance of thorough patient screening, both medically and psychosocially, as well as documenting decision making processes. It emphasizes aligning patient expectations through comprehensive education and informed consent procedures. The document also addresses issues like disclosing financial relationships, managing patient dissatisfaction, tracking complaints, conducting crucial conversations with difficult patients, and dismissing patients when needed. The overall message is that careful screening, education, documentation, and communication can help reduce the risk of legal claims.