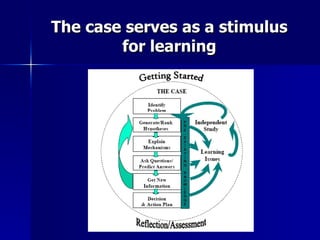
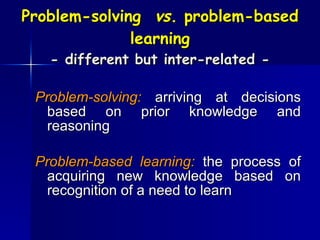
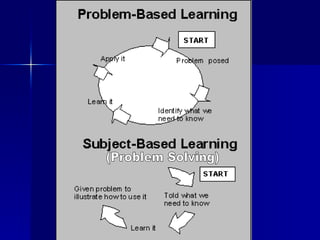
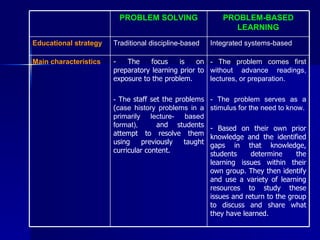
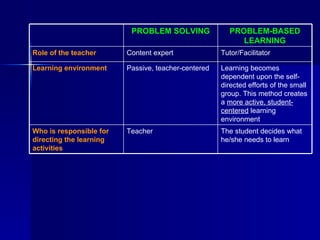
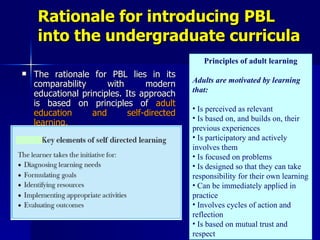
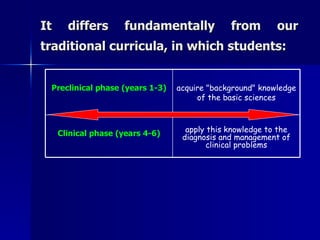
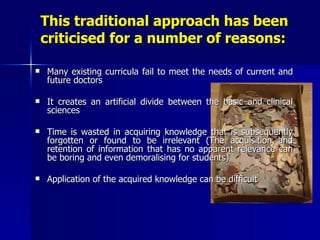
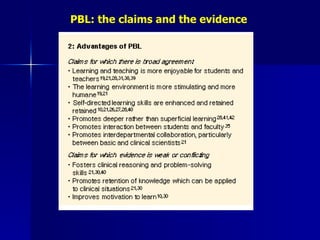
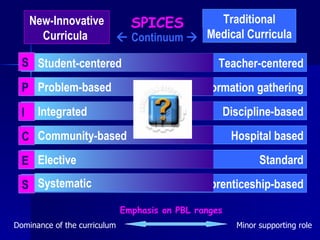
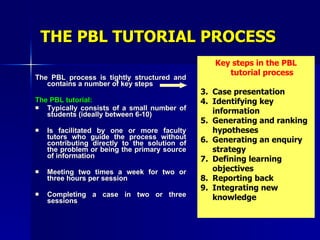
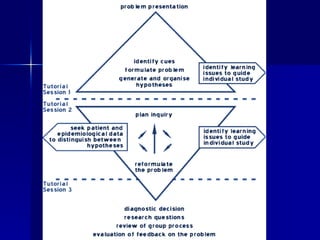
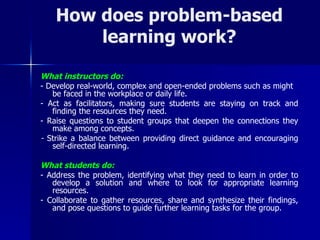
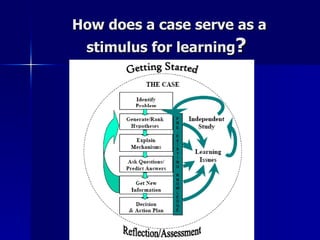
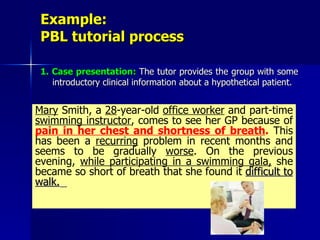
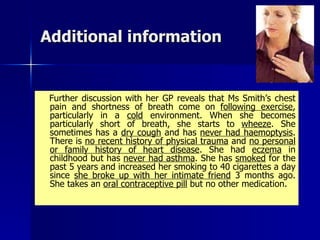
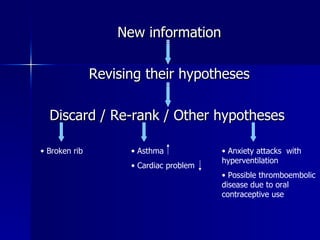
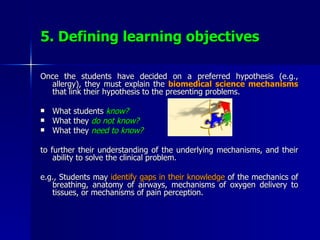
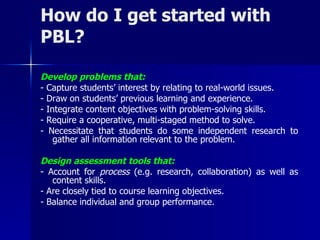
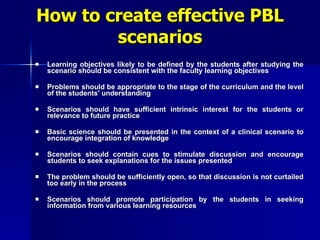
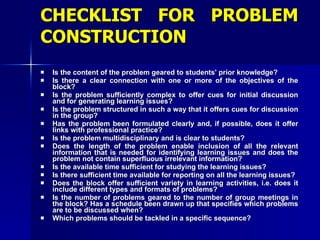
Problem-based learning (PBL) is a student-centered approach that uses clinical problems to stimulate learning. Students define their own learning objectives to address gaps in their knowledge. They then conduct self-directed study before reapplying their new knowledge to the problem. PBL differs from traditional lectures by making students responsible for their own learning through problem-solving in small groups with a tutor's guidance. Research shows PBL may better prepare students by integrating basic and clinical sciences and promoting long-term retention compared to traditional curricula.