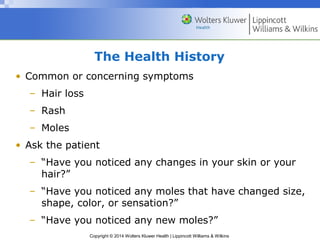
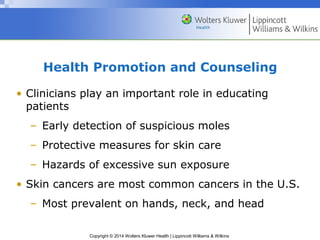
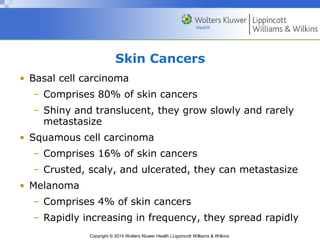
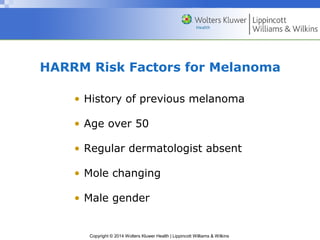
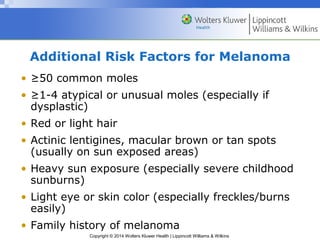
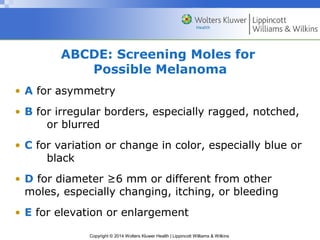
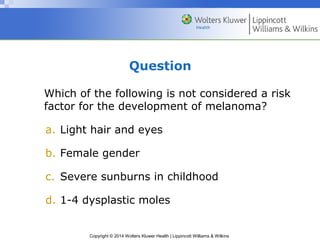
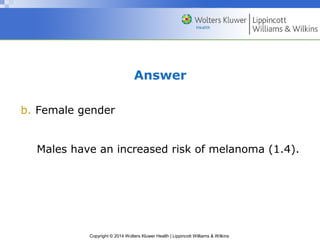
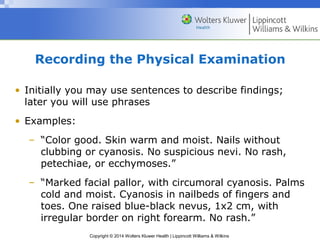
The document discusses the anatomy and examination of the skin, hair, and nails. It covers the major functions and layers of the skin, as well as the structure and types of hair and nails. Risk factors for skin cancers like melanoma are provided, along with techniques for examining the skin, hair, nails, and identifying lesions. Examination of bedbound patients and documenting findings are also reviewed.