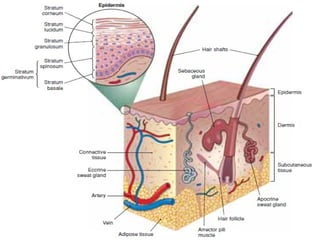
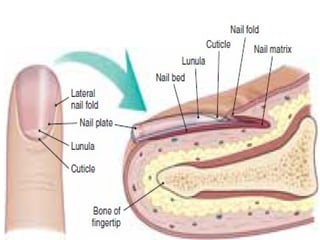
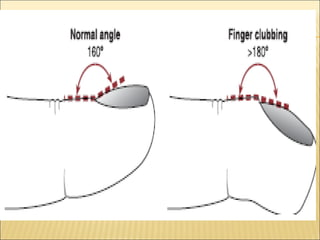
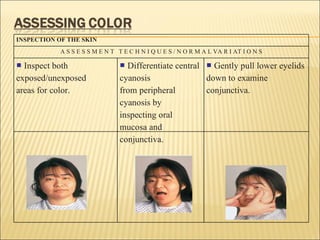
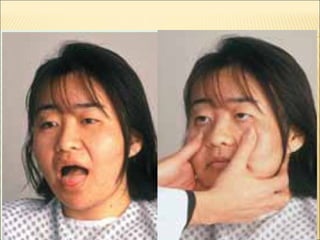
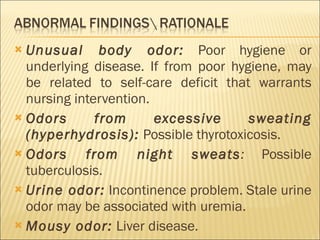
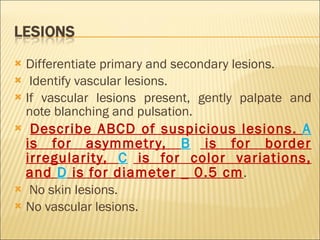
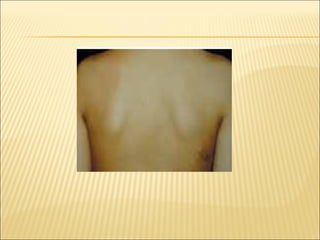
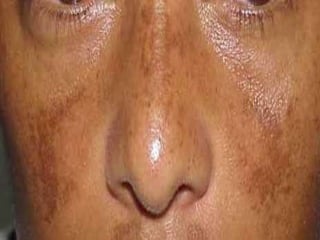
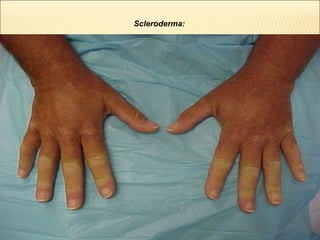
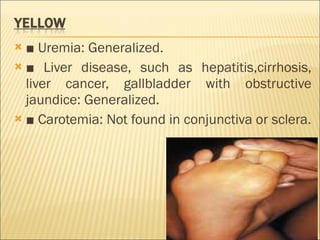
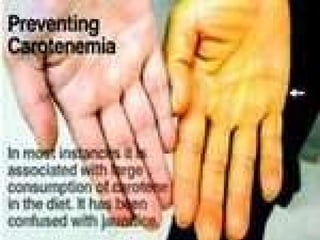
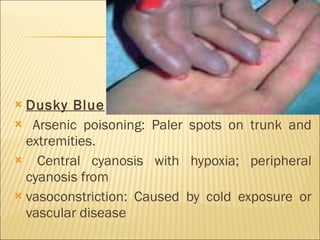
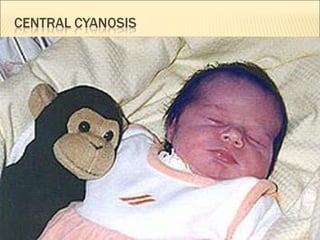
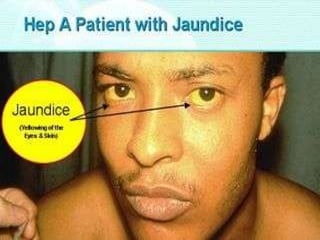
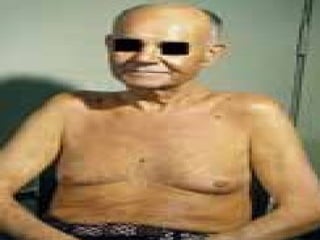
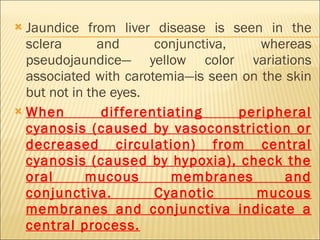
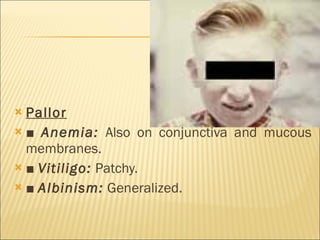
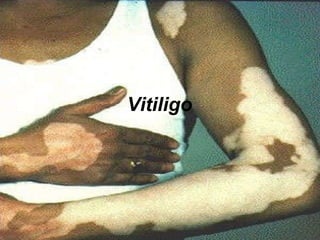
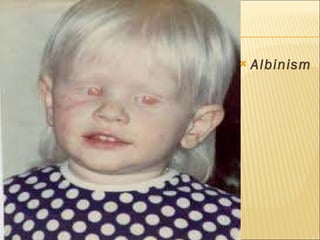
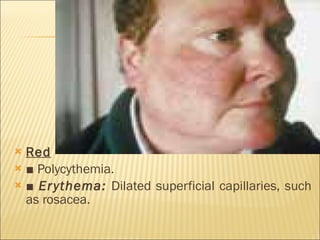
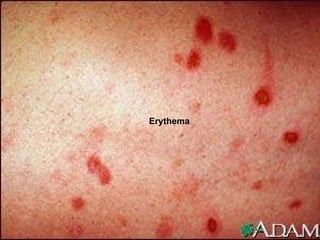
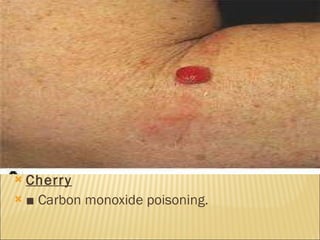
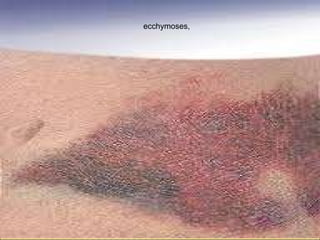
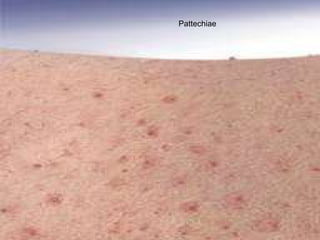
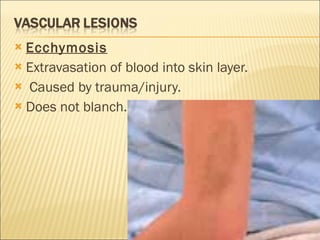
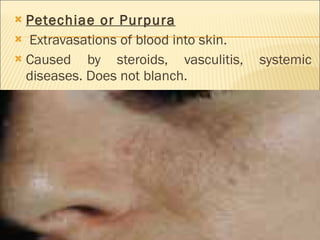
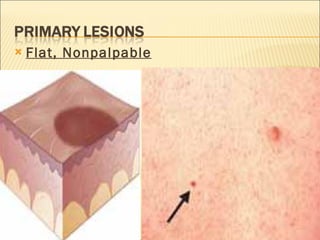
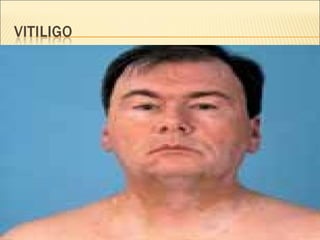
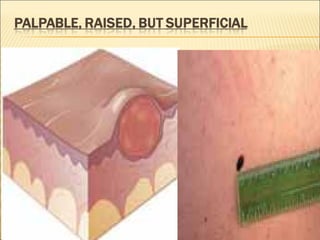
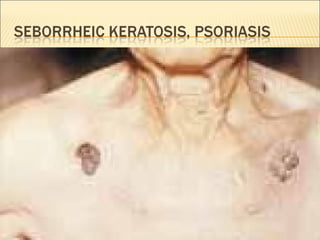
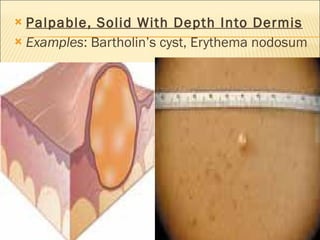
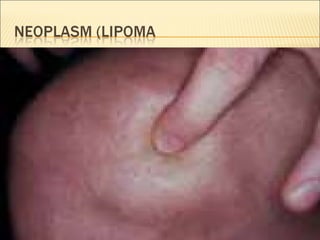
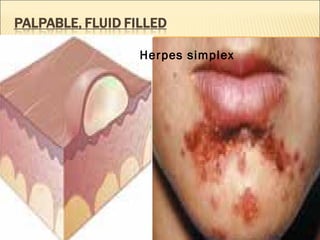
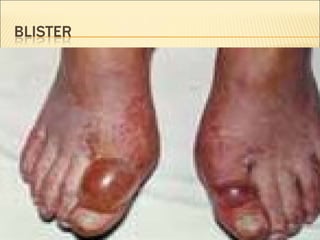
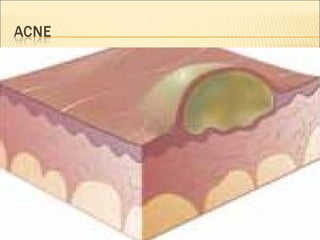
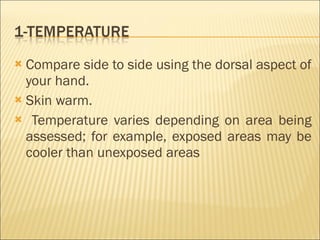
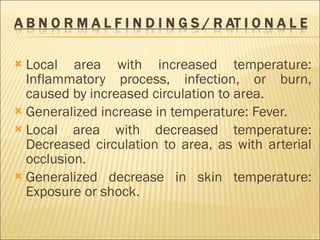
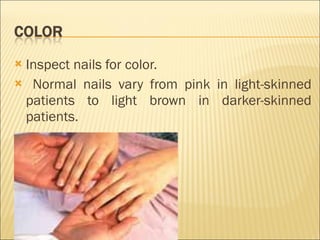
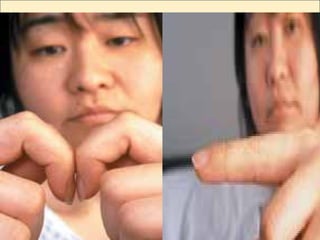
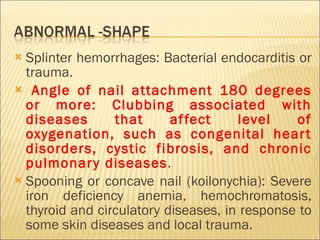
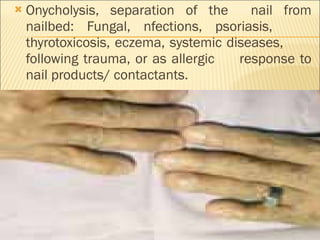
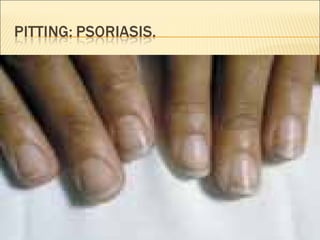
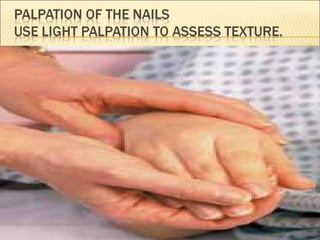
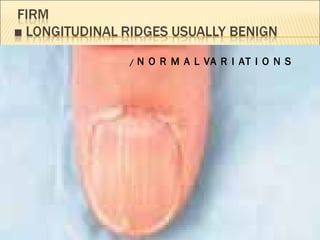
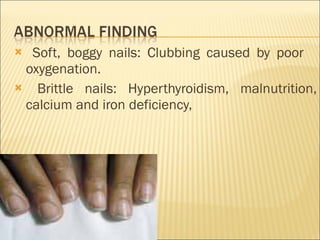
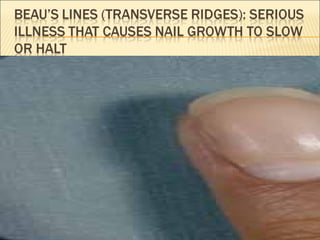
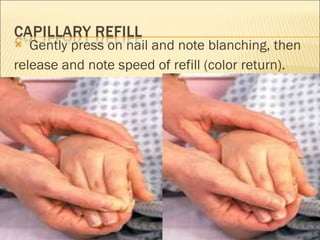
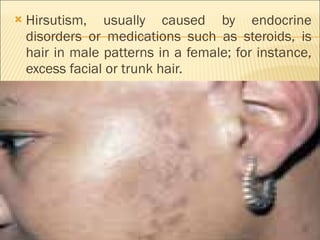
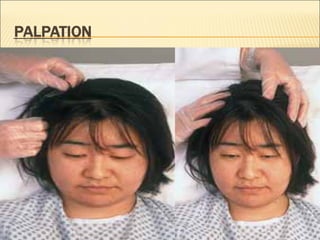
The document summarizes the key structures and functions of the integumentary system. It describes the layers of the skin, including the epidermis and dermis. It also discusses hair, nails, and glands. Assessment of the integumentary system involves inspection of the skin, hair, and nails to evaluate color, lesions, vascular changes, and other characteristics. Physical examination techniques include inspection and palpation.