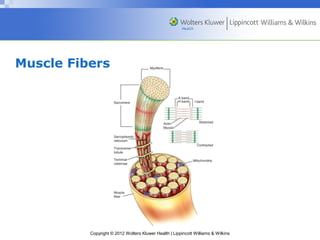
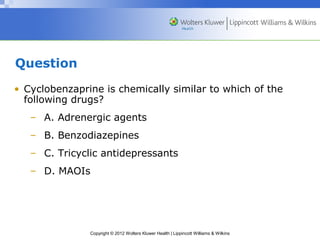
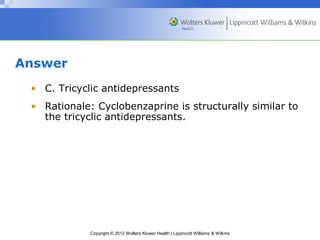
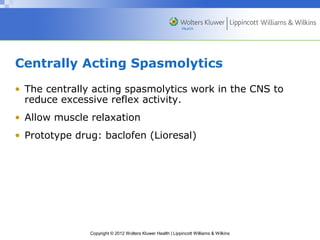
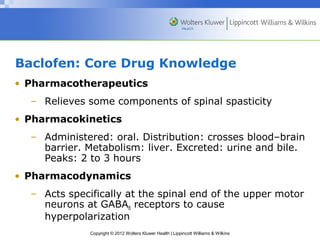
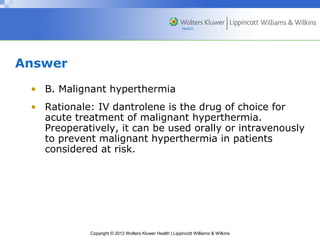
This document discusses drugs used to treat muscle spasm and spasticity. It begins by describing muscle physiology and the pathophysiology of muscle spasm and spasticity. It then describes two classes of drugs used to treat these conditions: centrally-acting muscle relaxants such as cyclobenzaprine which act in the central nervous system, and peripherally-acting spasmolytics such as dantrolene which act directly on skeletal muscles. For each drug, the document provides details on pharmacology, nursing considerations, teaching points, and potential adverse effects.