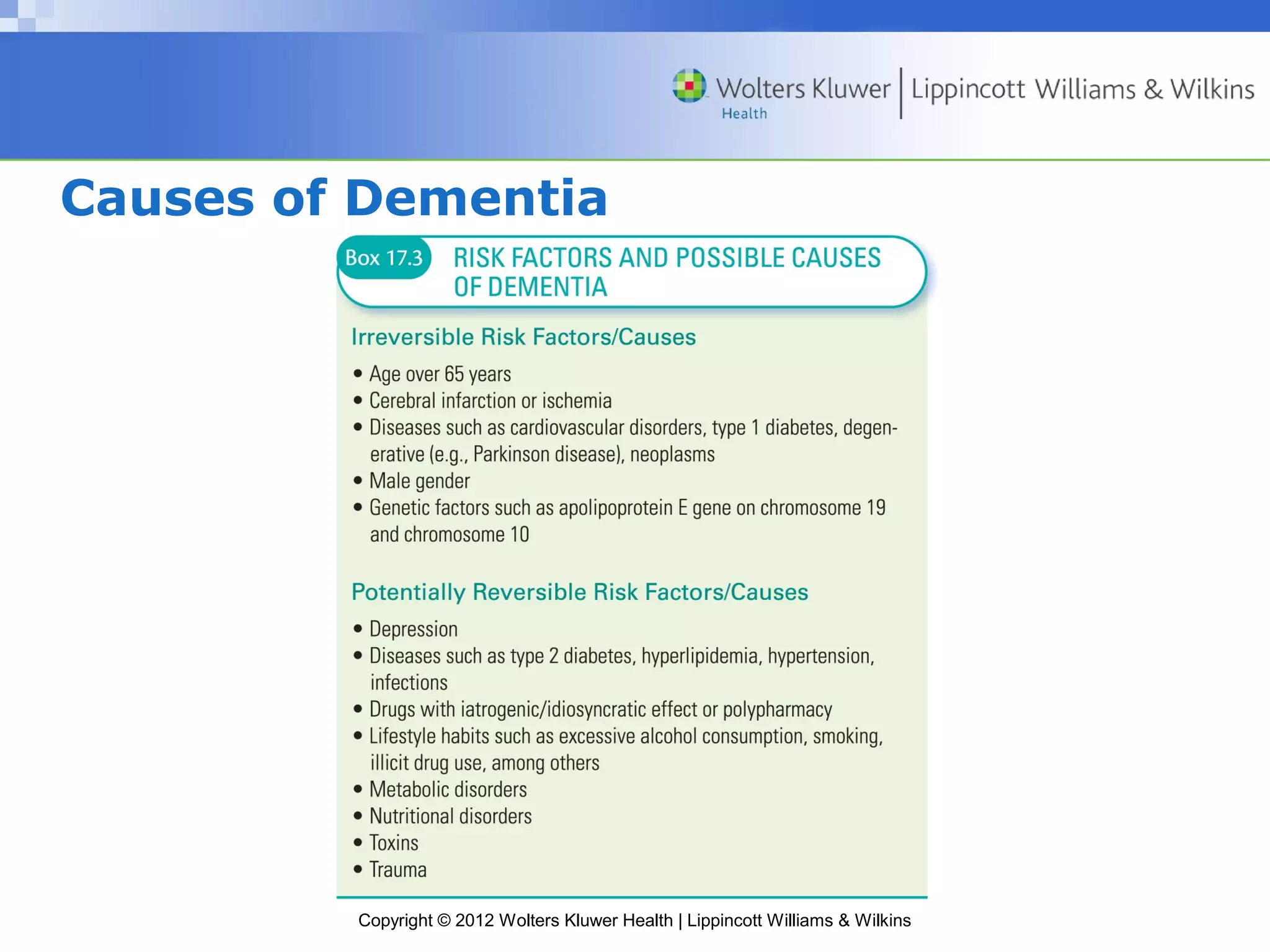
The document discusses drugs used to treat psychotic disorders and dementia. It covers the physiology of the brain and neurotransmitters like dopamine and acetylcholine. It then discusses specific conditions like schizophrenia, dementia, Alzheimer's disease, and vascular dementia. It describes typical and atypical antipsychotics used to treat psychosis, focusing on haloperidol and olanzapine. Side effects and nursing considerations are provided for monitoring and managing patients taking these drugs.