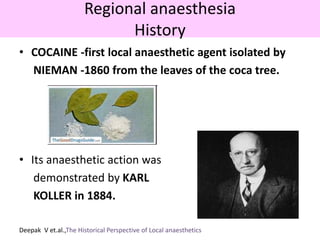
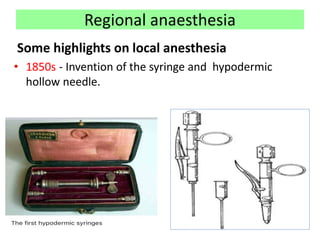
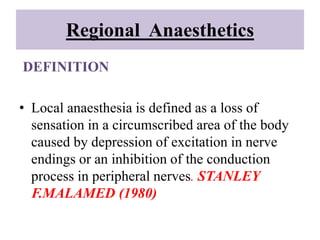
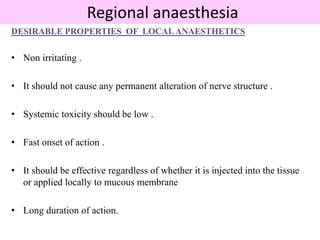
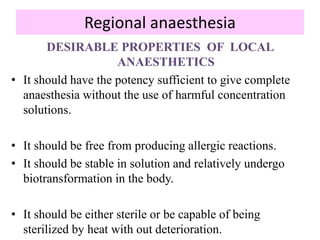
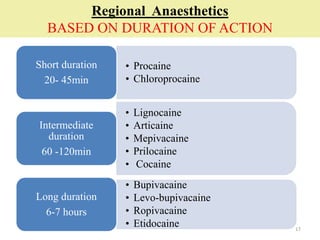
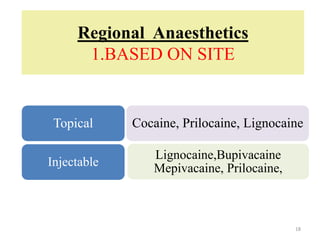
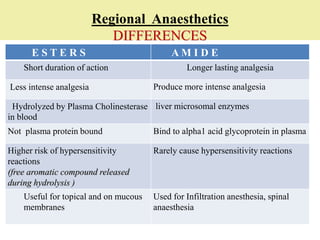
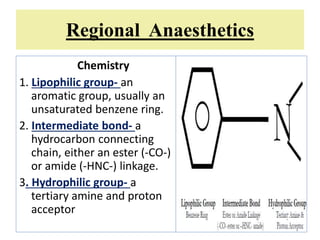
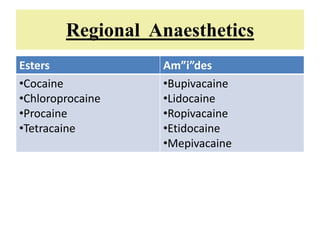
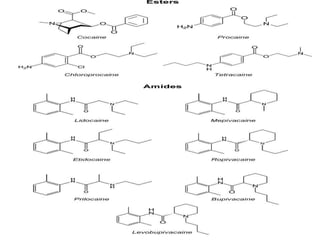
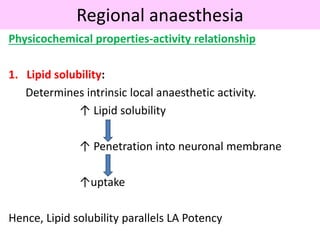
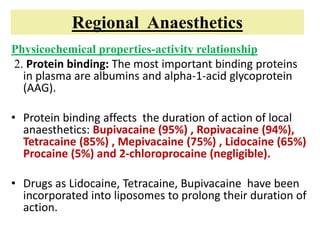
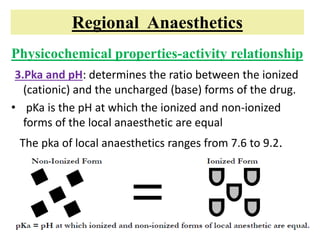
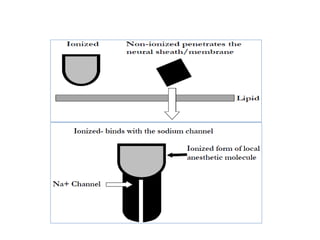
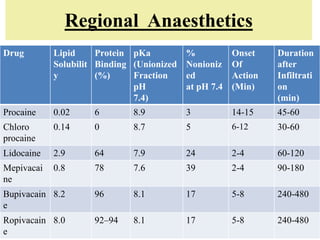
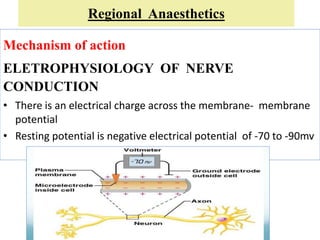
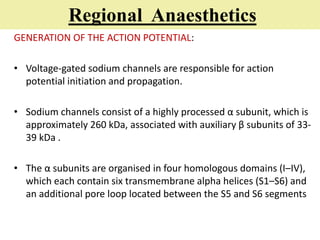
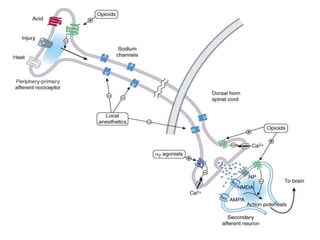
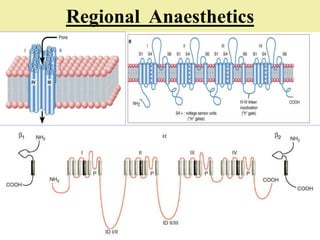
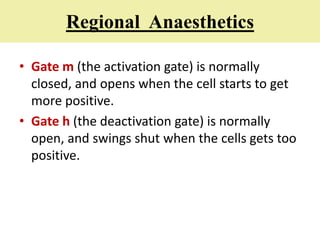
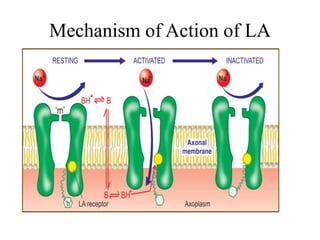
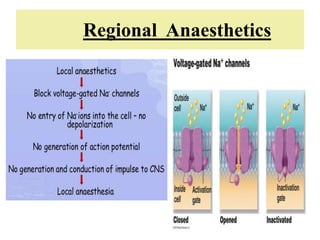
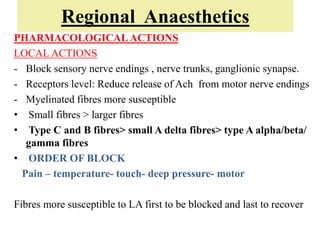
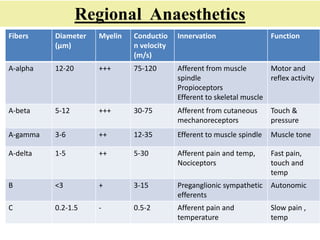
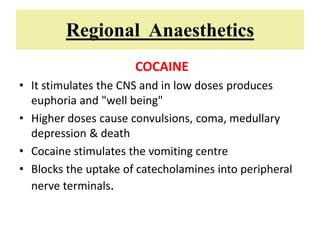
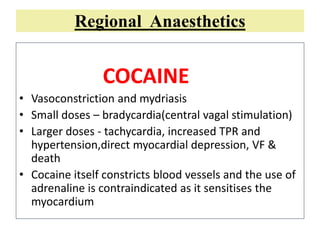
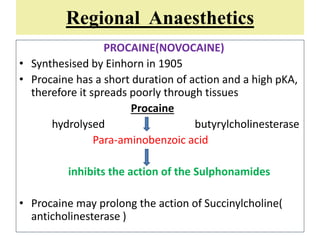
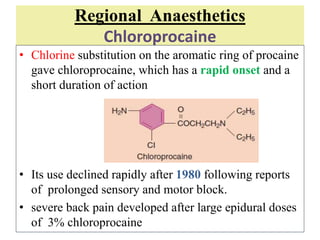
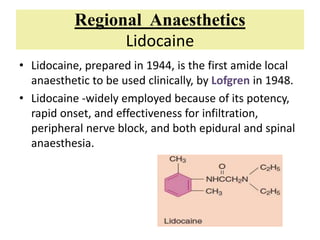
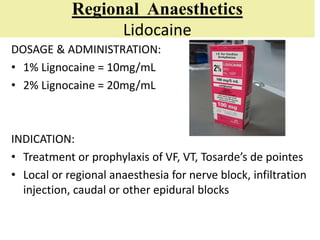
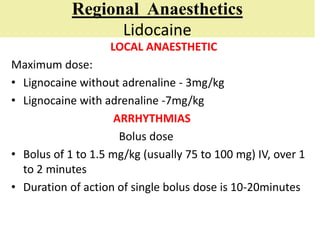
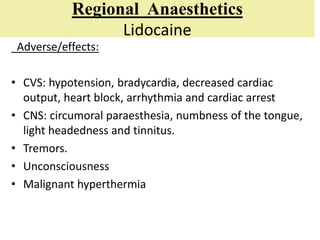
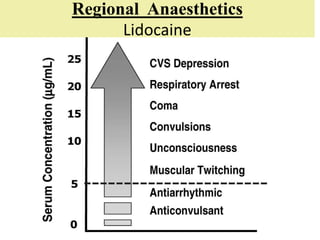
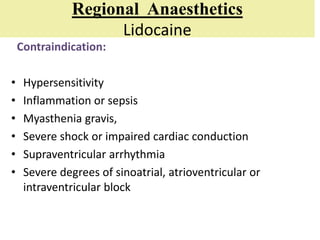
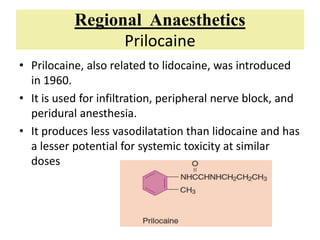
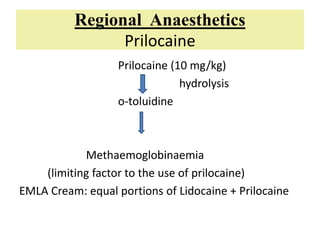
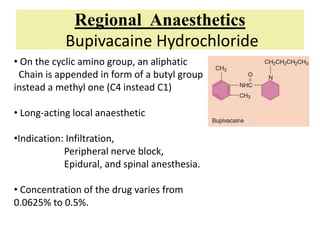
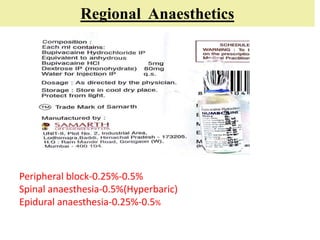
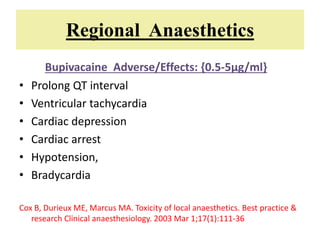
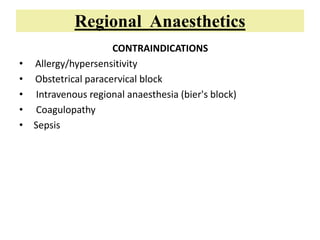
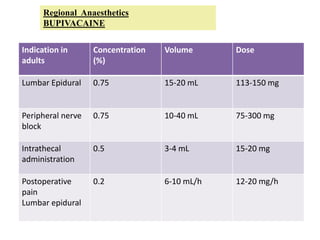
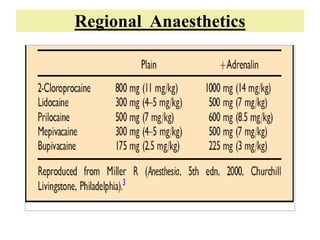
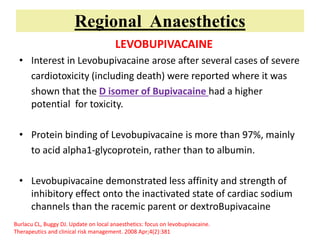
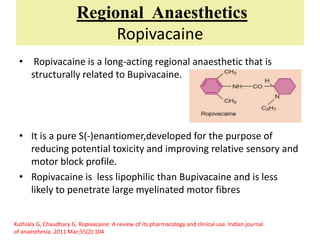
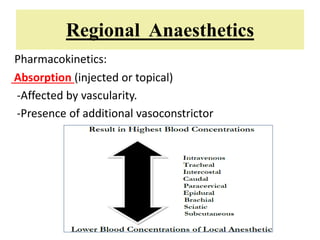
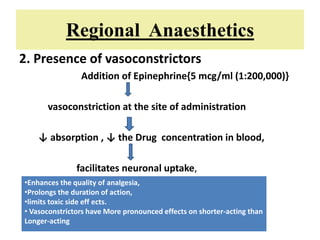
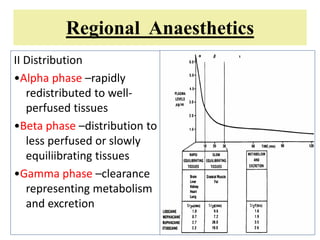
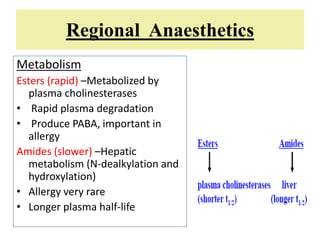
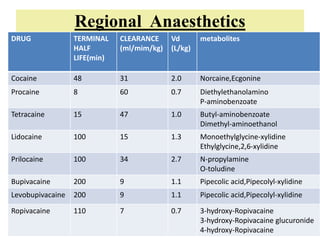
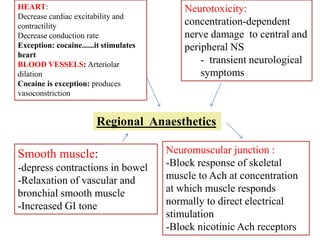
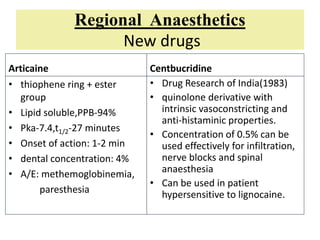
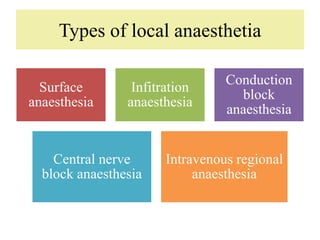
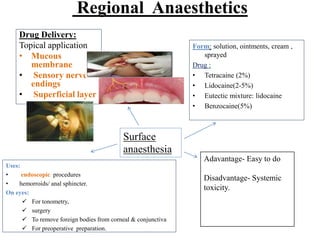
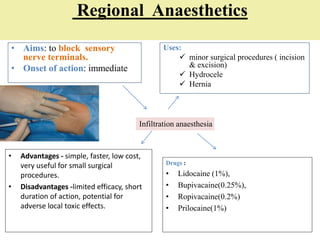
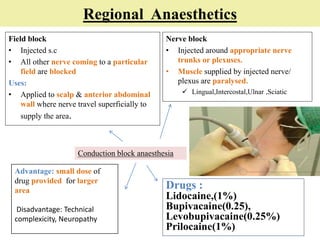
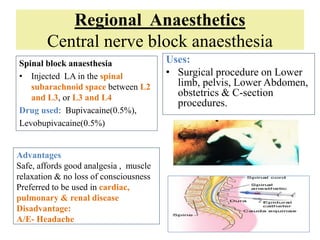
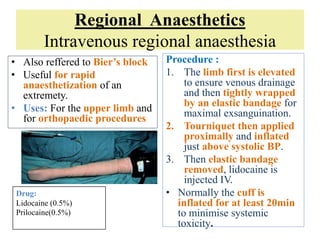
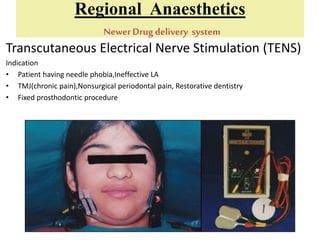
This document provides an overview of regional anaesthetics. It begins by defining regional anaesthesia as anaesthesia of a segment of the body through peripheral or neuraxial interruption of nerve transmission without loss of consciousness. The document then discusses the history of local anaesthetics from cocaine in the 1860s to modern agents like lidocaine and bupivacaine. It also covers the classification, mechanisms of action, pharmacological properties and therapeutic uses of various local anaesthetic agents.