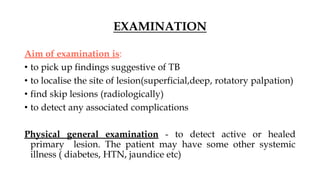
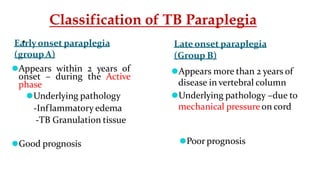
This document provides an overview of Pott's spine, including examination findings, differential diagnosis, complications, classification of paraplegia, treatment approaches, drug regimens, surgical indications and procedures, and spinal bracing options. The key points covered are the aims of examination to detect TB lesions and complications, common deformities and limitations seen, conservative and surgical treatment plans, first-line drug therapy including dosage, and types of spinal braces commonly used like the Milwaukee brace.