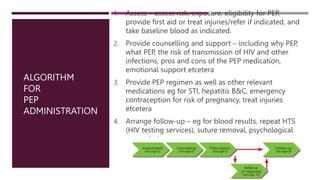
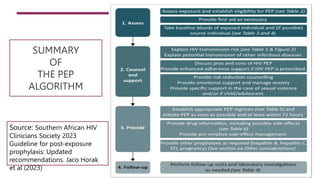
The document outlines the latest guidelines for HIV post-exposure prophylaxis (PEP) in South Africa, highlighting high rates of new infections, particularly among vulnerable populations. It explains the importance of PEP as an emergency intervention to prevent HIV acquisition within 72 hours of exposure, along with the administration algorithm and recommended regimens. Additionally, it emphasizes the role of holistic care and monitoring for side effects in promoting adherence to treatment.



![PEP ADMINISTRATION
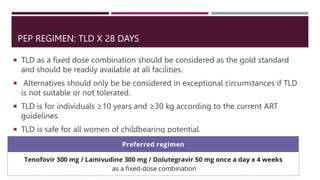
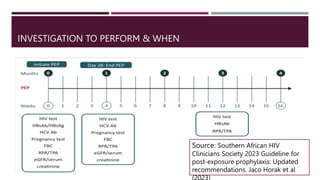
The global recommendation for PEP is a 3-drug regimen involving an
integrase inhibitor – usually dolutegravir
Integrase inhibitor-based regimens are very safe.
The recommended duration of a course of PEP is 28 days.
The full 28-day course should be provided at the time of PEP initiation.
The recommended regimen for PEP is now 28 days of first-line ART – i.e.,
tenofovir disoproxil, lamivudine anddolutegravir [TLD]
In instances of repeated PEP use in an individual, rather assess the potential
benefit of PrEPfor such an individual going forward.
Side effects must be monitored and managed appropriately to promote
adherence](https://image.slidesharecdn.com/postexposureprophylaxisbydrdele-231228065654-3312ca9d/85/Post-Exposure-Prophylaxis-by-Dr-Dele-17-320.jpg)