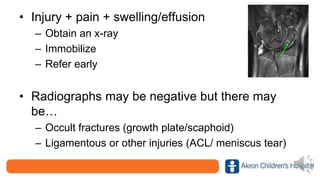
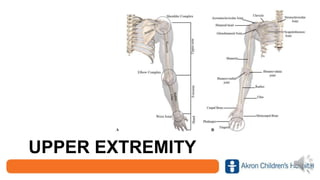
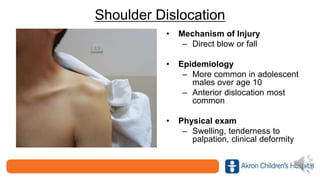
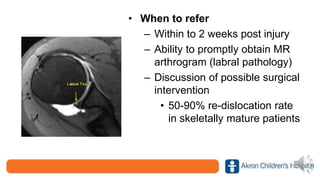
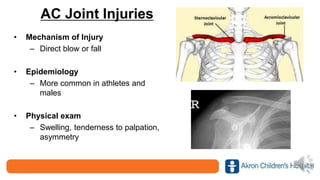
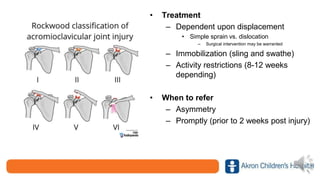
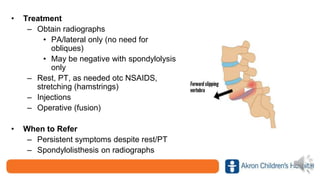
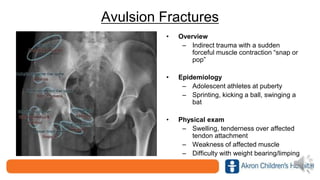
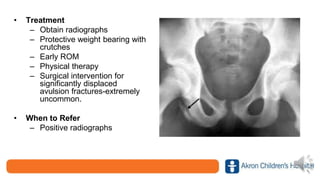
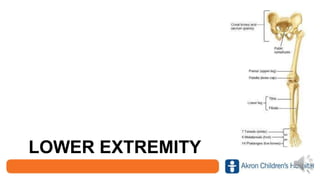
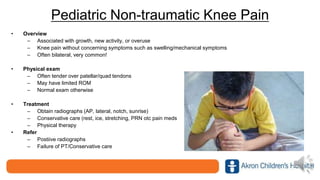
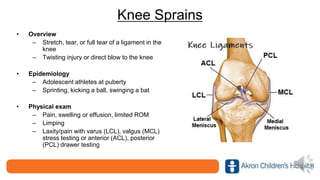
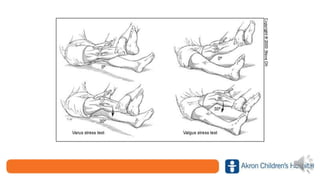
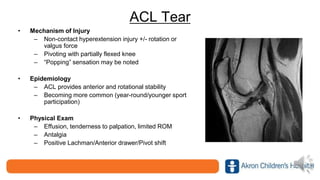
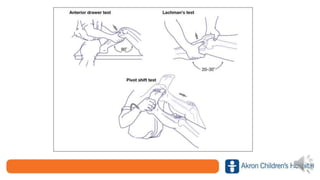
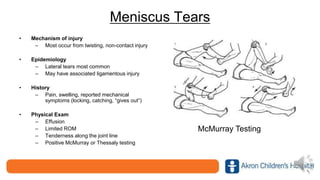
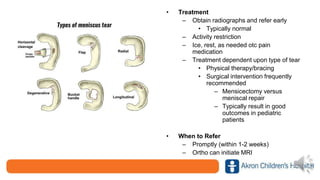
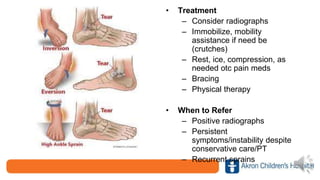
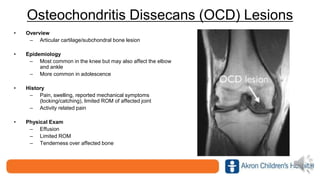
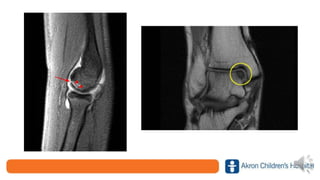
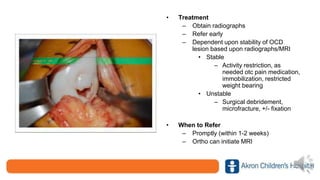
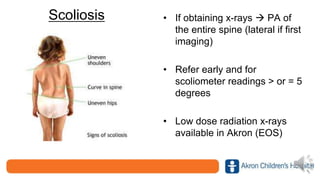
This document provides guidance on recognizing and managing common pediatric sports injuries. It discusses injuries of the upper extremity including shoulder dislocations, AC joint injuries, clavicle fractures, Little League shoulder, and finger injuries. For the lower extremity, it covers knee sprains, ACL tears, meniscus tears, ankle sprains, and osteochondritis dissecans lesions. It emphasizes the importance of early referral for injuries like ACL tears. Key referral criteria mentioned include persistent symptoms despite rest/physical therapy and positive radiographic findings. Clinical pearls provided include obtaining x-rays for injuries with pain, swelling and effusion and recognizing that not all injuries are just sprains.