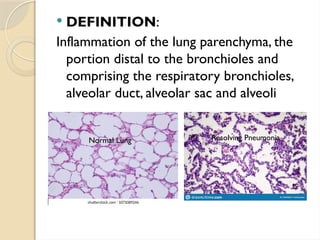
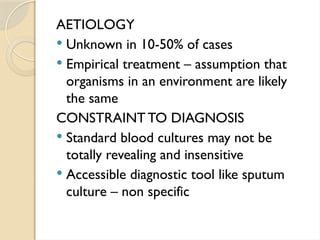
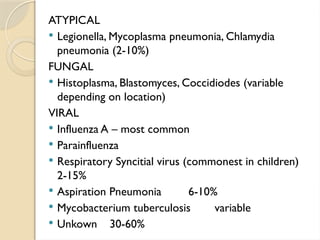
The document provides a comprehensive overview of pneumonia, including its definition, epidemiology, causes, and classification by anatomical and pathological criteria. It discusses the clinical features, diagnostic approaches, treatment options, and potential complications associated with pneumonia, as well as specific characteristics of various pneumonia-causing organisms. Additionally, it highlights risk factors, predisposing conditions, and methods for assessing severity in patients.