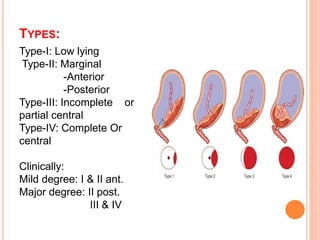
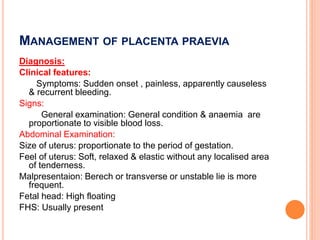
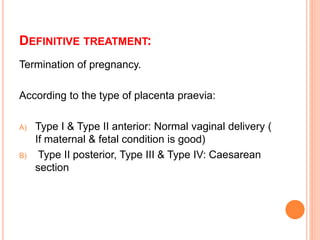
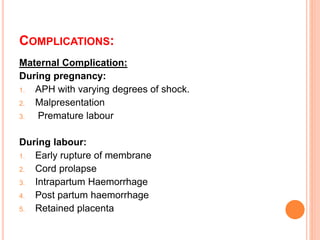
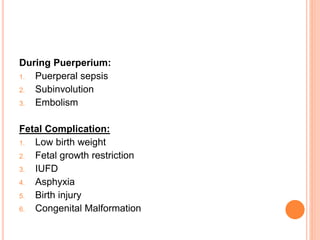
This document discusses placenta praevia, which is when the placenta implants partially or completely over the lower uterine segment. It notes the causes and risk factors, types, characteristics of bleeding, management including expectant treatment and definitive treatment depending on the type, and complications for both mother and baby. The presentation was given by Dr. Bijit Talukdar and covered the topic of placenta praevia in detail.