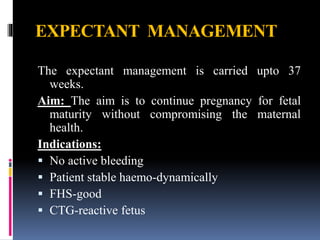
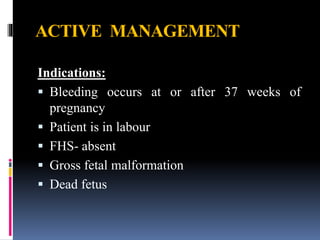
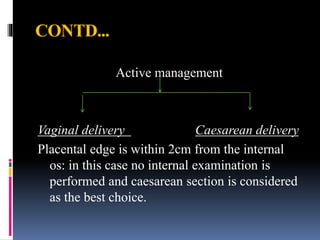
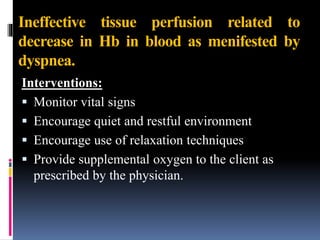
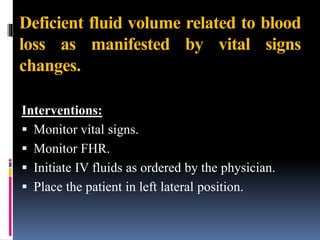
Placenta praevia is a condition where the placenta is implanted in the lower uterine segment, either partially or completely covering the internal cervical os. There are four types depending on the degree of coverage of the cervical os. It can cause painful vaginal bleeding and is a risk factor for preterm birth and fetal complications. Diagnosis is made using ultrasound and careful examination. Management involves bed rest, monitoring for bleeding, and delivery via c-section if bleeding occurs late in pregnancy or labor begins. Nursing care focuses on monitoring for signs of decreased blood volume and tissue perfusion.