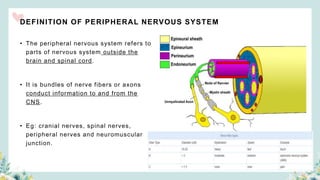
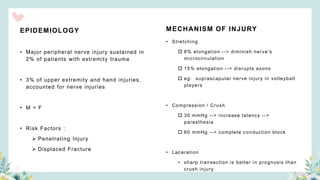
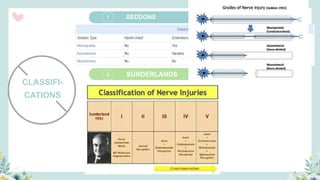
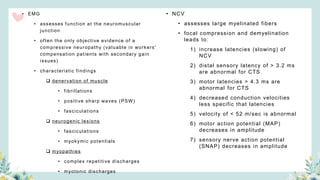
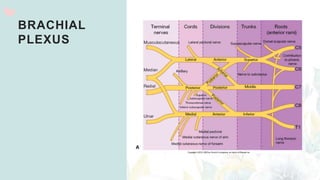
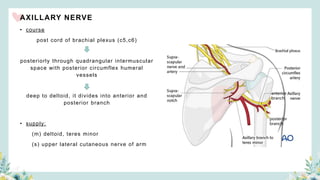
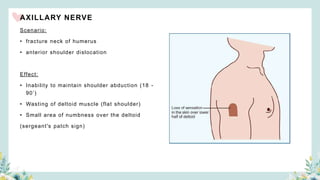
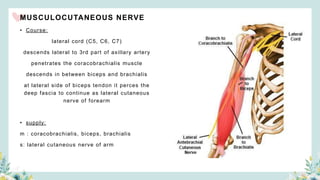
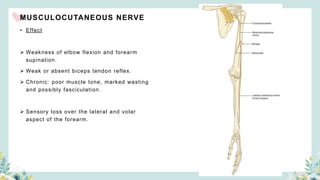
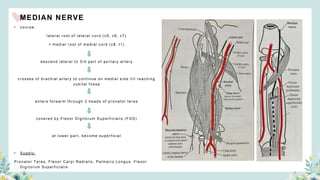
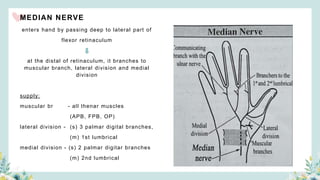
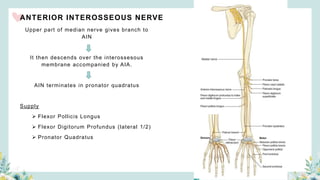
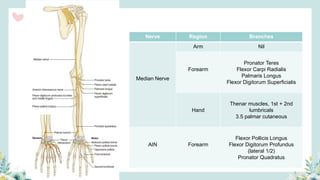
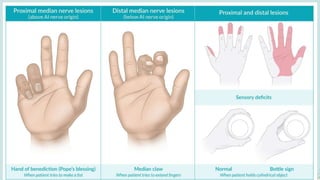
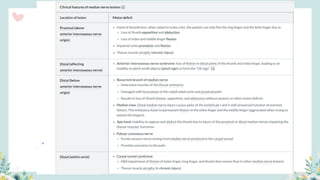
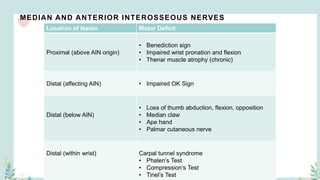
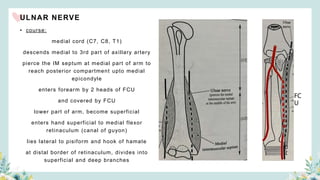
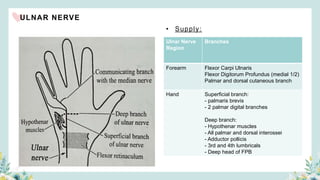
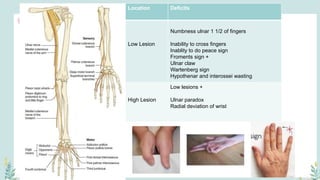
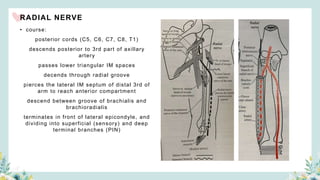
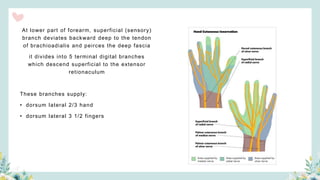
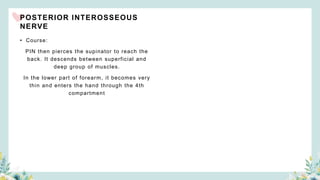
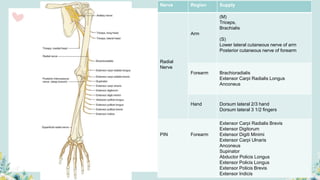
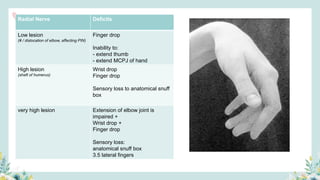
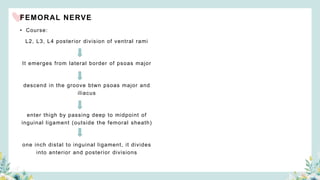
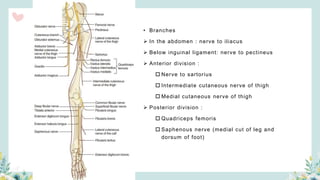
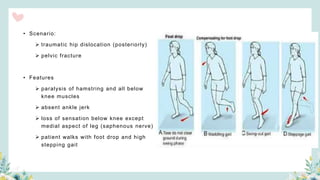
Peripheral nerve injuries can occur due to stretching, compression, or laceration of nerves outside of the brain and spinal cord. These injuries are commonly caused by trauma or fractures and can result in numbness, weakness, or paralysis depending on the specific nerve affected. Peripheral nerve injuries are often classified by severity and investigated using electromyography and nerve conduction studies. Treatment may involve splinting, rehabilitation, or surgical repair depending on the nature of the injury. Common specific nerve injuries include brachial plexus injuries, median and ulnar nerve injuries, and injuries to the radial, femoral, and sciatic nerves.