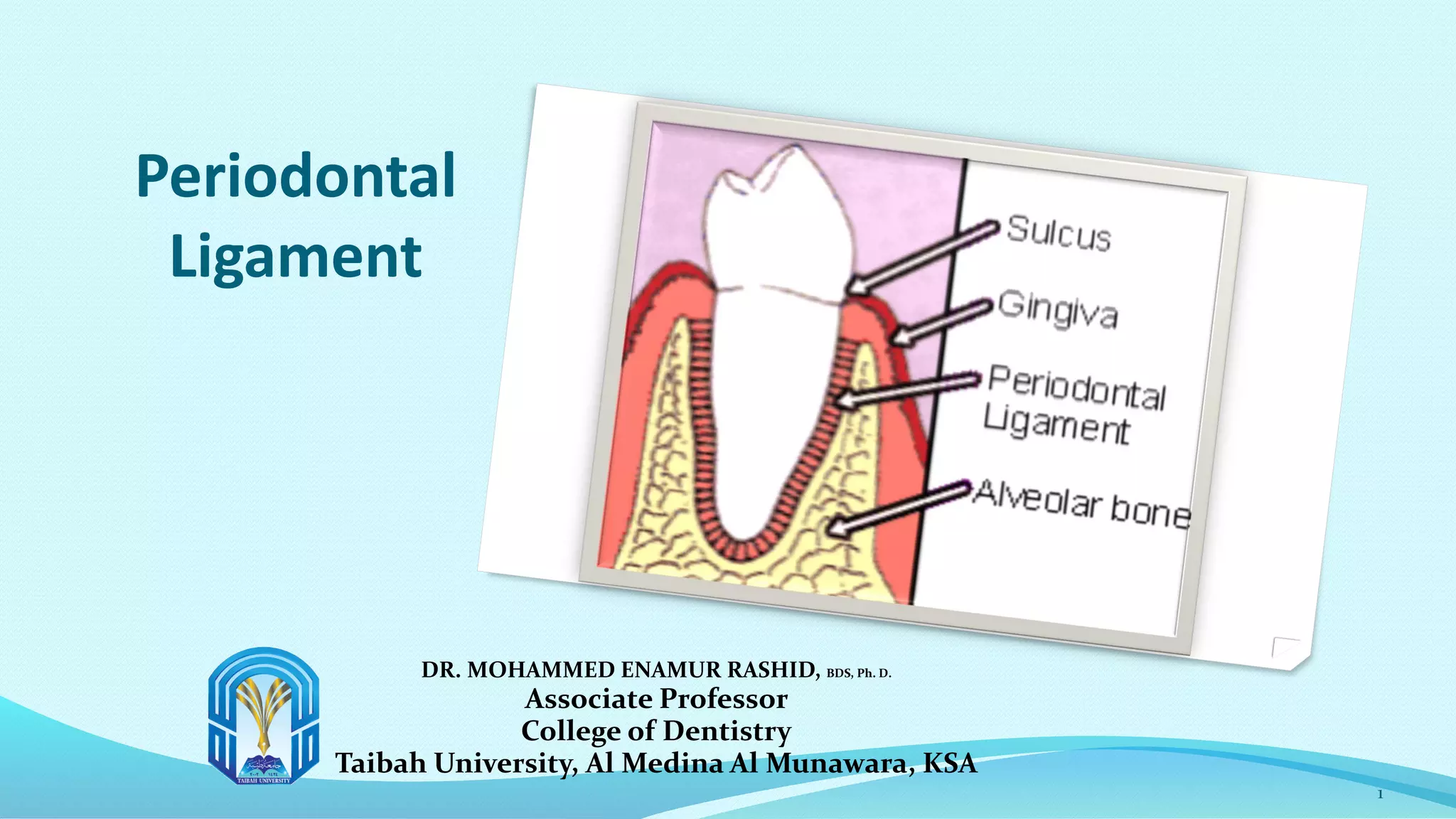
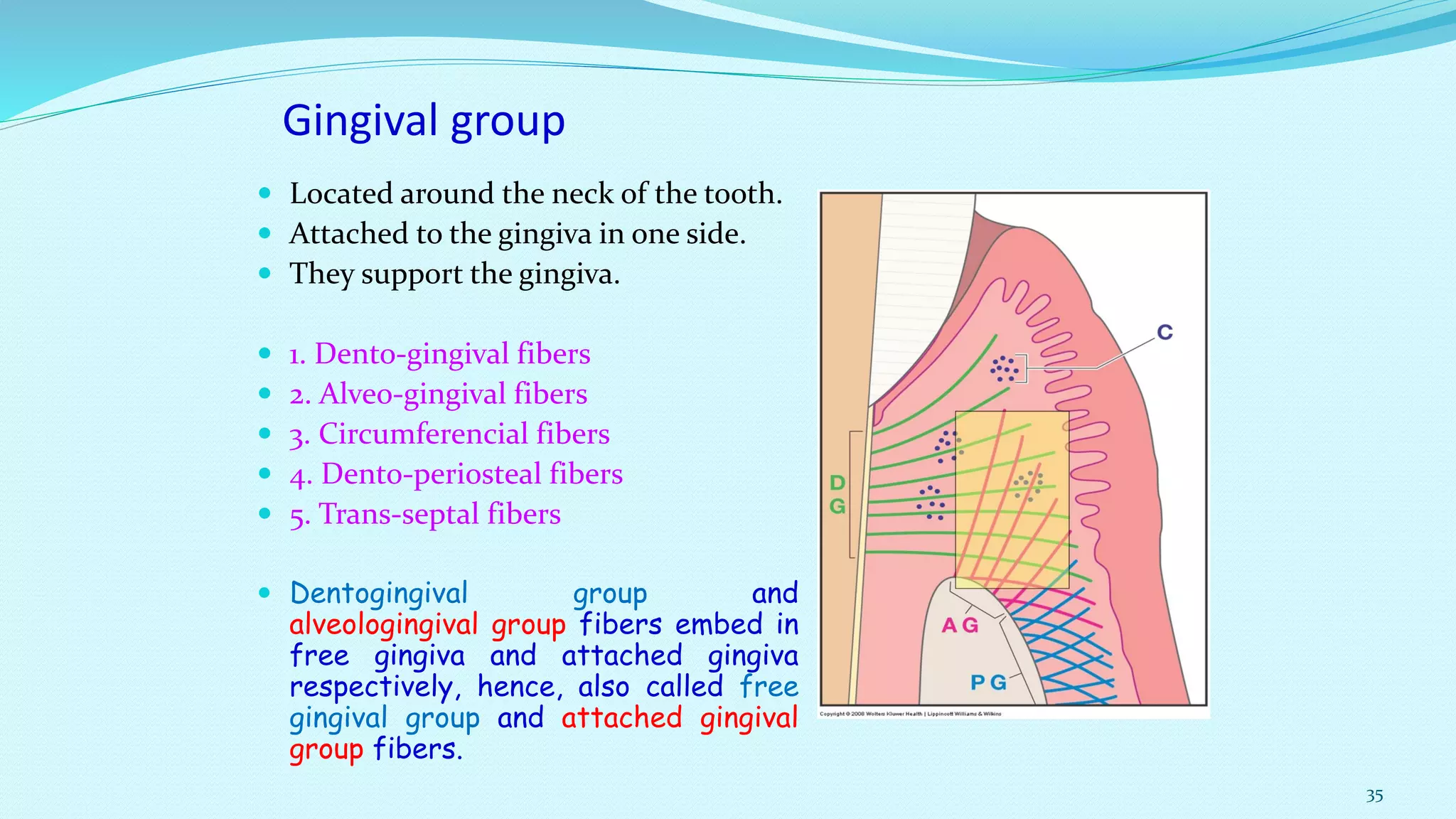
The periodontal ligament is a fibrous connective tissue that attaches the tooth to the alveolar bone. It is composed of fibers, cells, blood vessels and ground substance. The fibers are arranged in bundles that provide support, resist displacement, and allow movement. The principal fiber groups include gingival fibers around the neck of the tooth and dento-alveolar fibers along the root. Blood supply comes from the superior and inferior alveolar arteries.