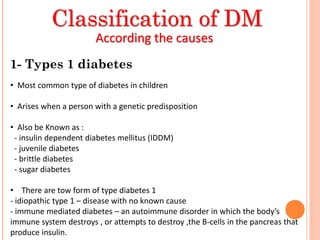
The most common type of diabetes in children and teens is type 1 diabetes, also called juvenile diabetes. With type 1 diabetes, the pancreas does not produce insulin. Type 2 diabetes used to be called adult-onset diabetes but is becoming more common in children due to increases in obesity. Children with type 2 diabetes are at high risk if they are overweight, have a family history of diabetes, or are not physically active. Lifestyle changes like maintaining a healthy weight, being physically active, eating smaller portions of healthy foods, and limiting screen time can lower the risk of type 2 diabetes in children. Children with type 2 diabetes may be managed through diet and exercise alone, but some patients will need oral medications or insulin. Children with type