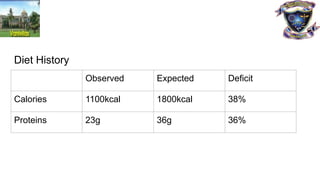
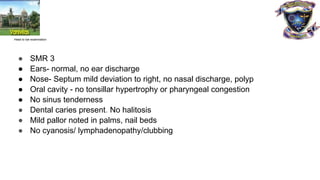
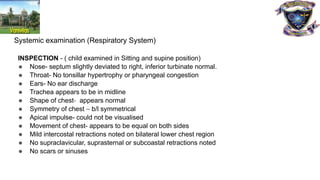
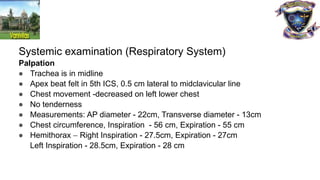
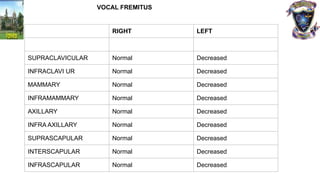
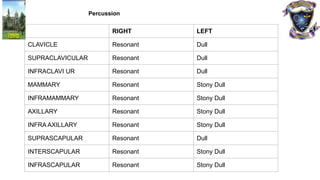
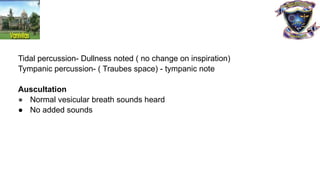
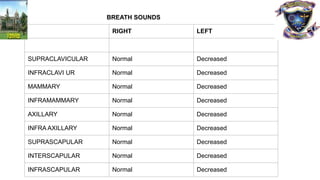
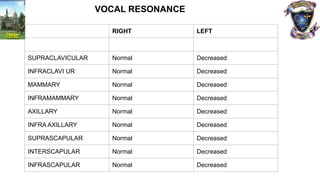
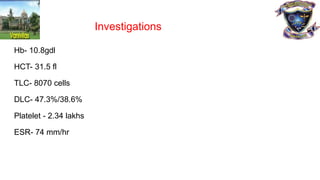
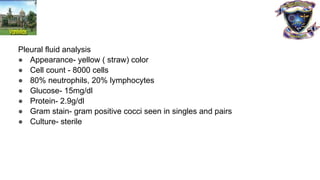
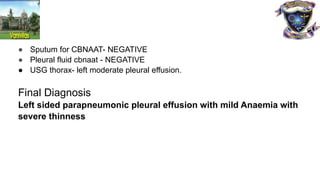
A 9-year-old female child presented with a 15-day history of chest pain, fever, cough, and hurried breathing. Clinical examination suggested left-sided pleural effusion likely secondary to a bacterial infection, with significant respiratory distress and severe thinness. Investigations confirmed the presence of pleural effusion and moderate anemia, leading to a final diagnosis of left-sided parapneumonic pleural effusion.