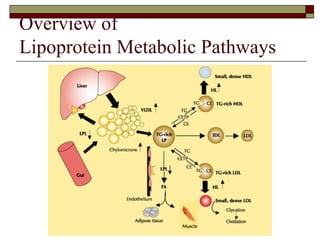
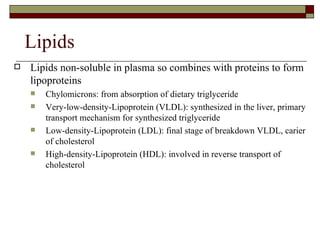
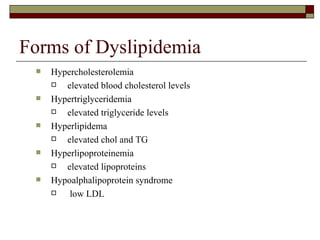
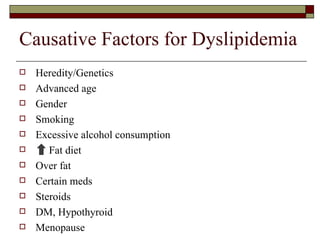
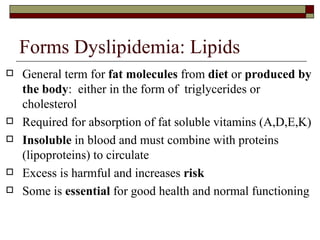
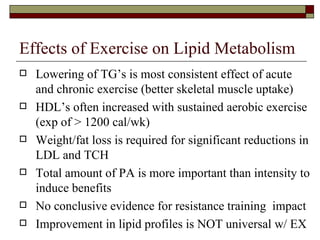
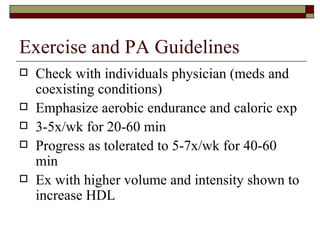
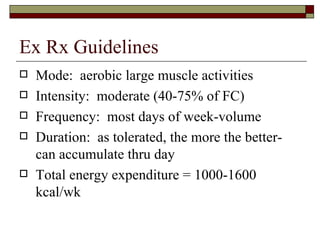
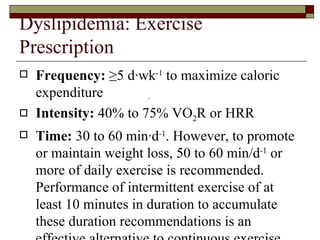
Dyslipidemia refers to abnormal blood lipid or lipoprotein levels and is linked to increased risk of cardiovascular disease. It involves high levels of triglycerides and/or cholesterol, which circulate in the bloodstream within lipoprotein particles. Lifestyle factors like diet, physical activity, smoking, and alcohol can influence lipid levels. Regular aerobic exercise of moderate intensity for 30-60 minutes per day at least 5 days per week is an effective way to improve lipoprotein profiles through increased calorie expenditure and weight control, particularly by raising HDL levels and lowering triglycerides.