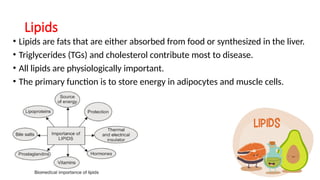
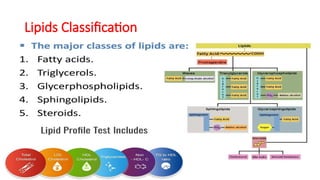
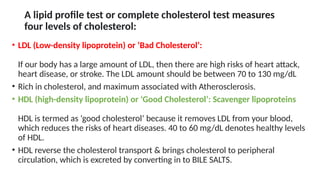
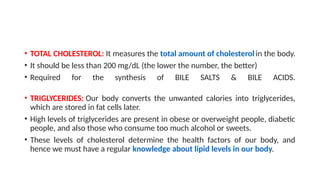
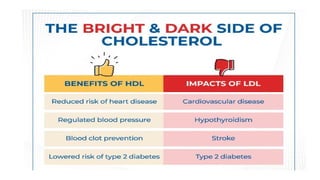
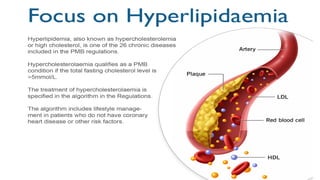
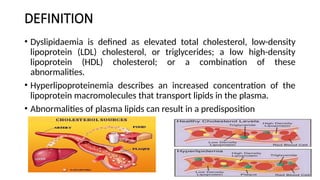
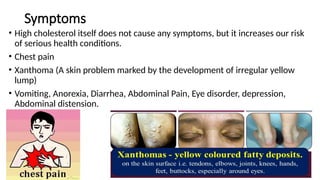
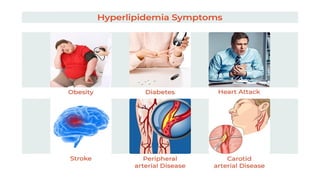
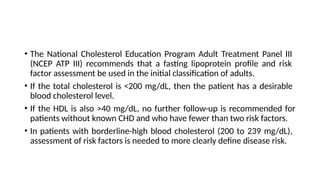
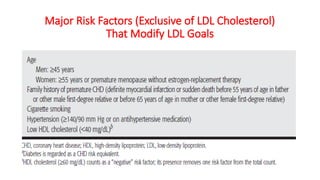
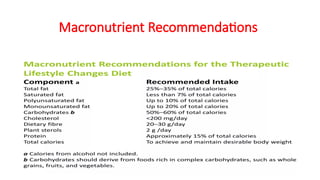
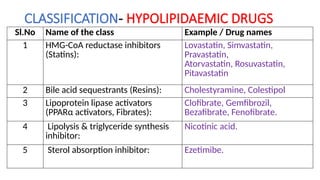
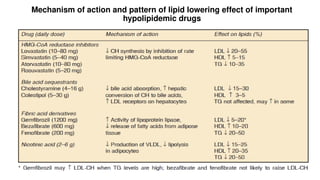
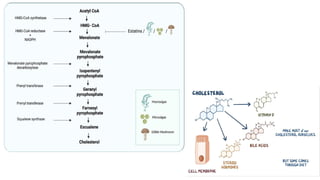
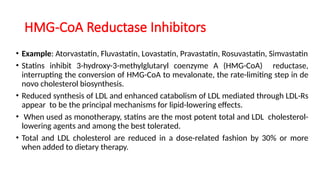
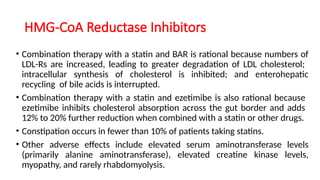
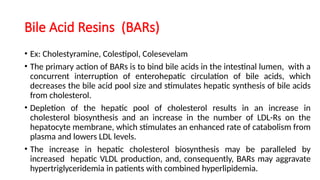
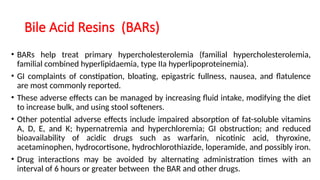
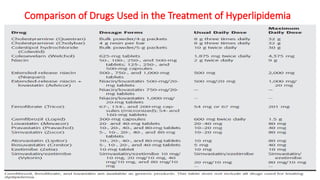
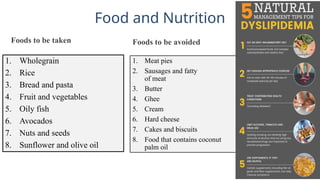
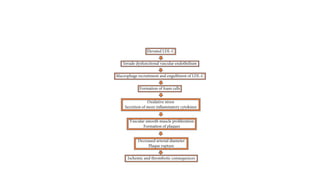
The document discusses the pharmacotherapeutics of hyperlipidaemia, including definitions, epidemiology, causes, and treatment options. It emphasizes the importance of maintaining healthy lipid levels through non-pharmacological and pharmacological treatments, monitoring lipid profiles, and addressing lifestyle factors such as diet, exercise, and smoking cessation. The document also details various classes of hypolipidaemic drugs and their mechanisms of action in lowering cholesterol levels.