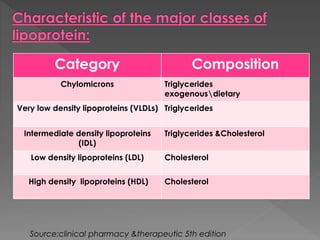
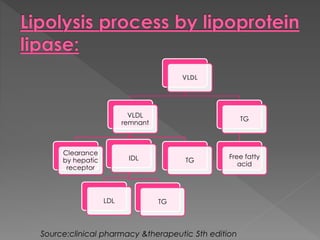
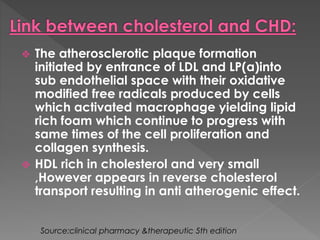
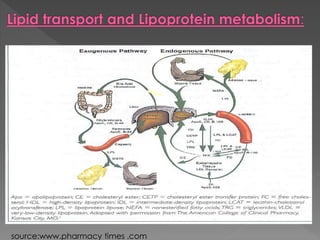
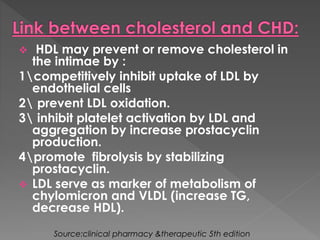
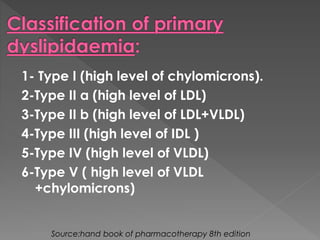
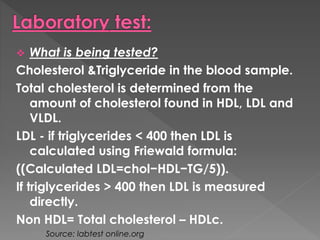
The document discusses cholesterol and lipoproteins. It states that cholesterol is essential for cell membrane structure and steroid hormone production. Cholesterol is transported through the body bound to lipoproteins including chylomicrons, VLDLs, IDLs, LDLs, and HDLs. Chylomicrons carry dietary cholesterol from the intestines through the lymphatic system before breaking down into chylomicron remnants that are taken up by the liver. The liver produces VLDLs that circulate and break down into LDLs, which are the major cholesterol carriers. High LDL levels increase risk of cardiovascular disease. HDLs aid in reverse cholesterol transport and have a protective effect against cardiovascular disease.