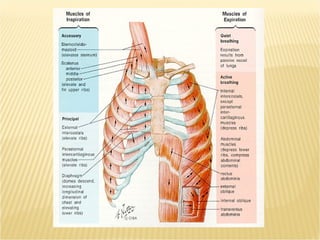
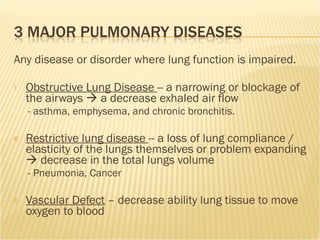
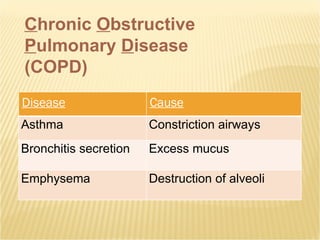
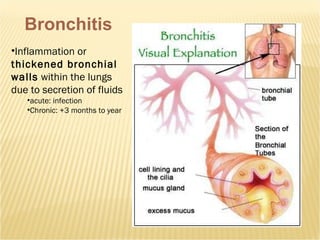
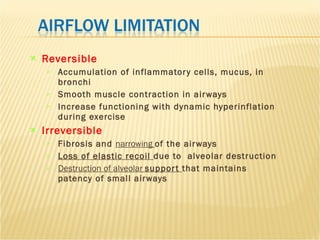
The document discusses pulmonary system function and exercise limitations caused by pulmonary diseases. It covers topics like pulmonary ventilation, diffusion, and different types of pulmonary diseases including chronic obstructive pulmonary disease (COPD), asthma, bronchitis, and emphysema. It provides guidelines for exercise for those with pulmonary impairment, focusing on intensity, duration, monitoring symptoms, and addressing complications of pulmonary diseases.