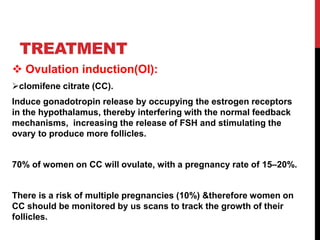
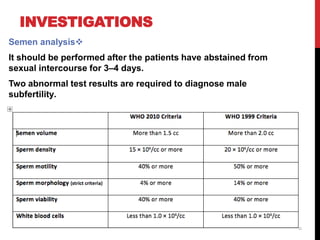
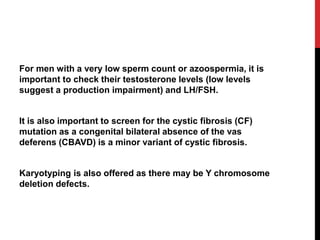
Subfertility is defined as the inability to conceive after 12 months of unprotected intercourse, with specific evaluation timelines based on female age. Various factors affecting fertility include age, lifestyle choices, hormonal imbalances, and anatomical issues, leading to different classifications such as primary and secondary subfertility. Treatments range from ovulation induction to advanced techniques like IVF and surgical interventions, with considerations for both male and female causes of infertility.