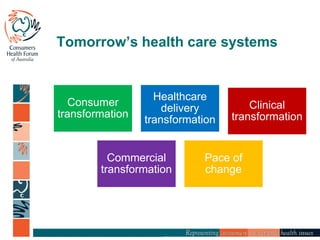
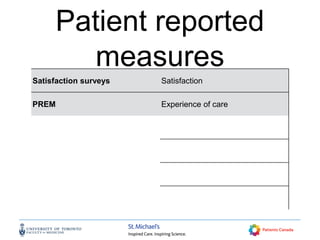
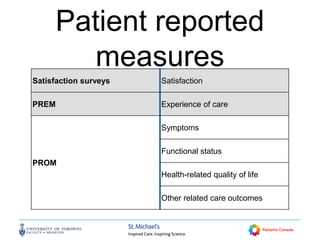
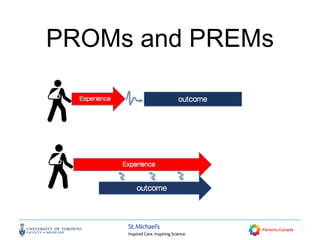
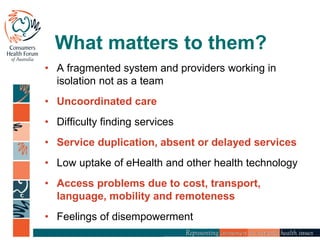
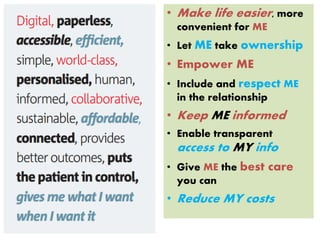
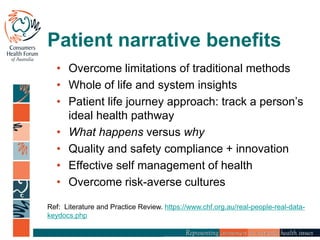
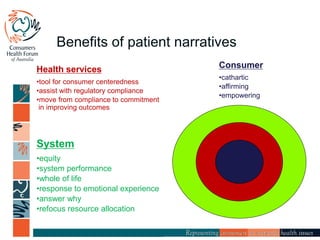
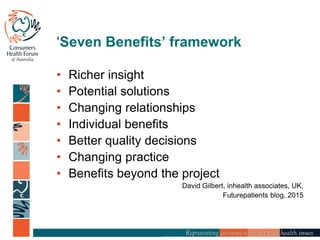
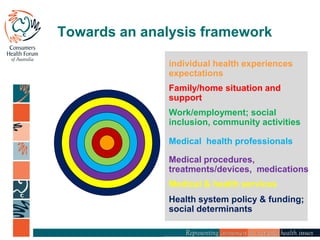
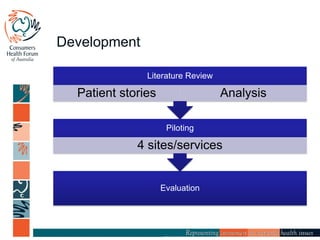
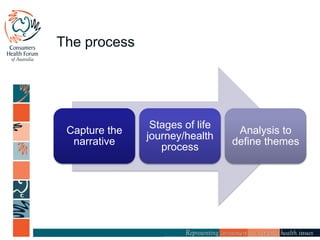
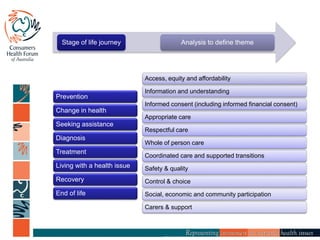
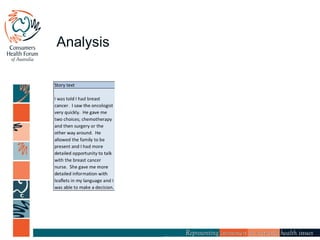
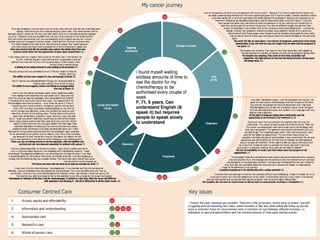
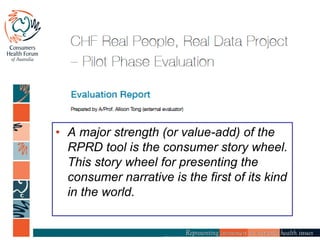
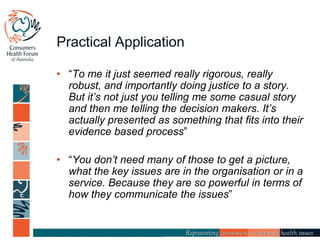
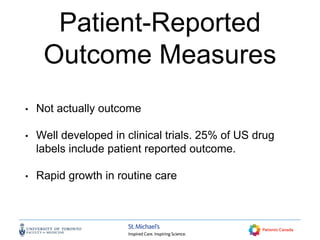
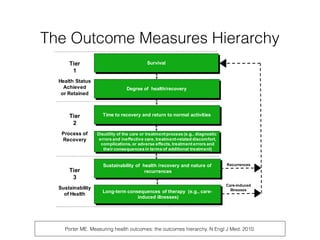
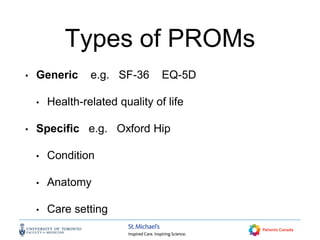
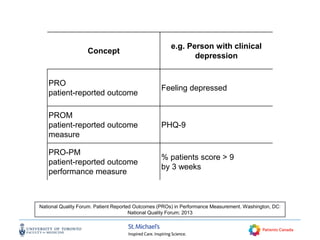
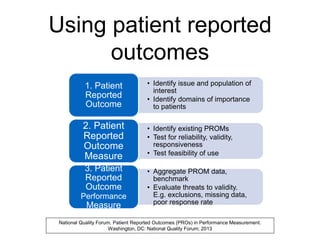
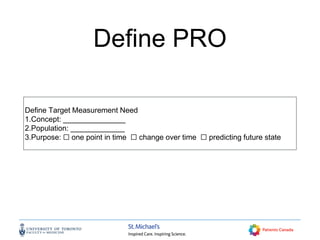
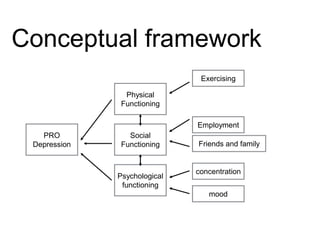
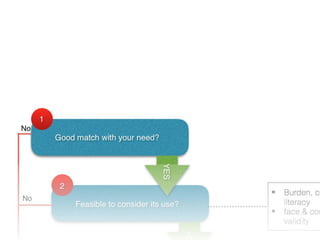
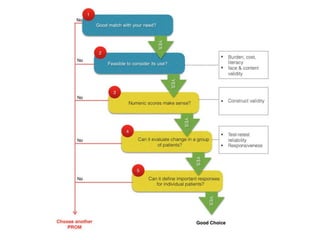
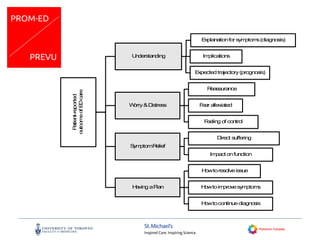
The document discusses the development and importance of patient-reported outcome measures (PROMs) in healthcare systems, emphasizing their role in improving patient care quality and engaging patients in their health narratives. It highlights the use of the 'real people, real data' tool to capture comprehensive patient experiences and facilitate better outcomes through understanding individual health journeys. The session outlined includes insights from various experts on the use of PROMs, patient engagement, and strategies for healthcare transformation focused on delivering value to patients.