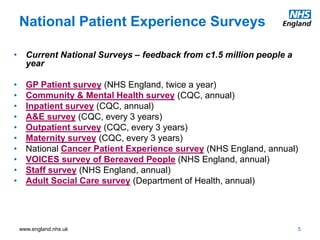
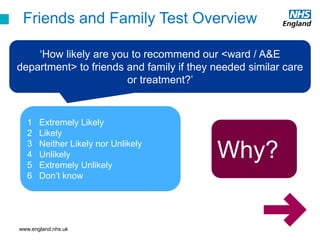
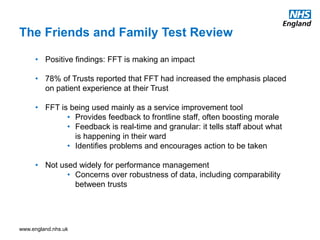
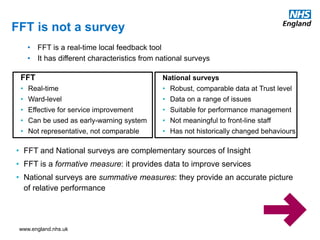
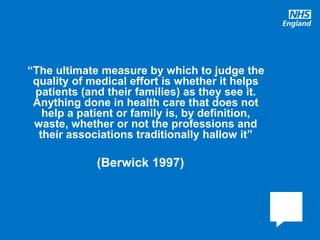
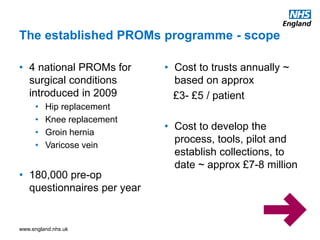
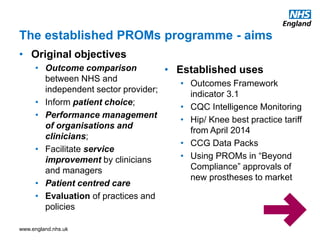
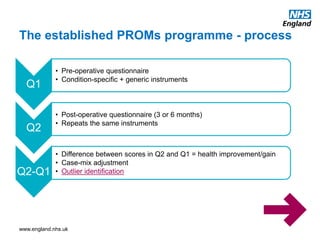
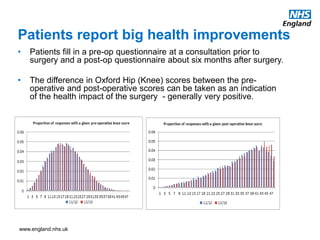
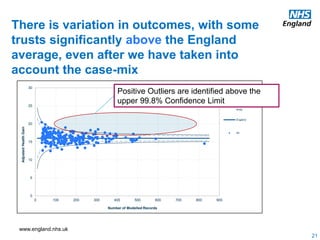
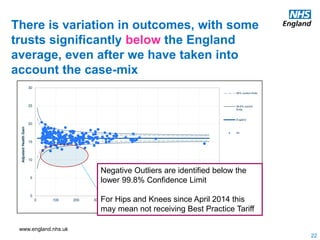
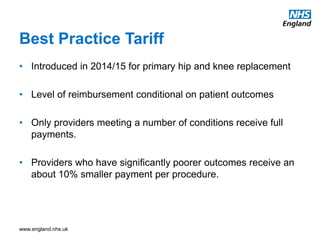
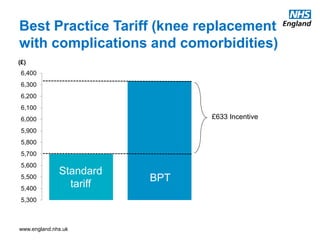
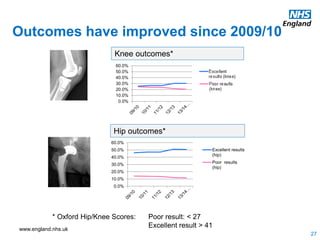
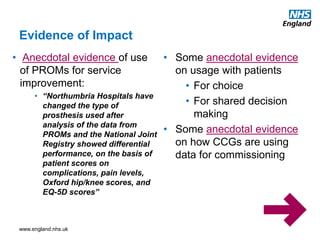
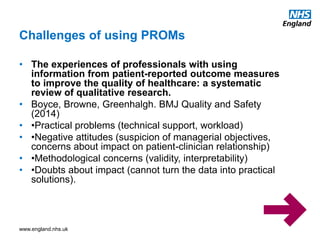
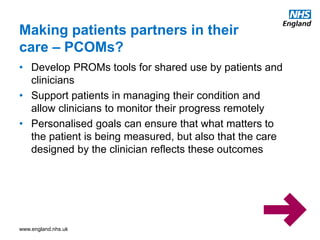
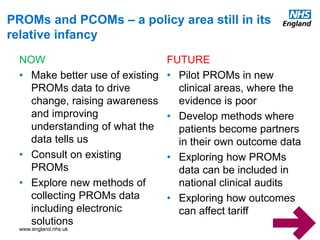
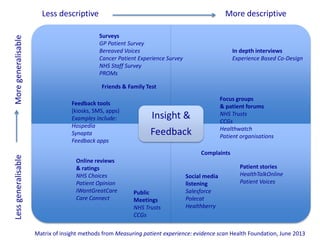
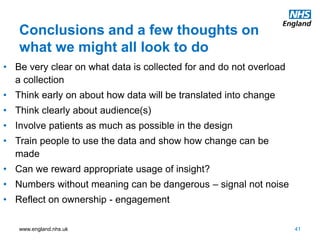
This document summarizes NHS England's approach to gathering patient experience and outcome data. It discusses various data collection methods, including national patient surveys, the Friends and Family Test, and Patient Reported Outcome Measures (PROMs). It notes that PROMs data shows patients report significant health improvements after surgeries and there is some variation in outcomes between hospitals. The document also outlines challenges in using this data and opportunities for the future, such as developing new PROMs for additional clinical areas and engaging patients more in collecting and using their own outcome data.