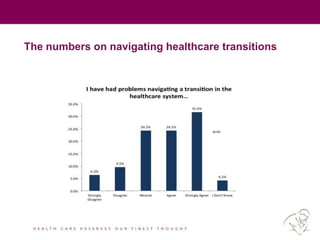
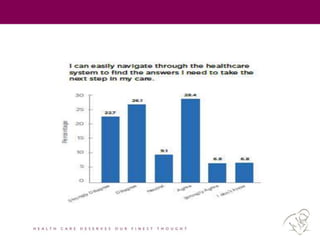
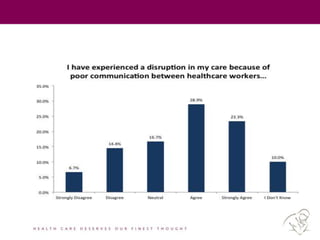
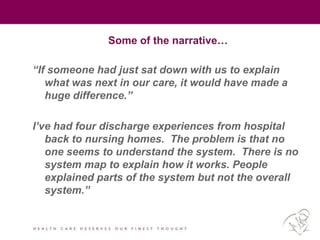
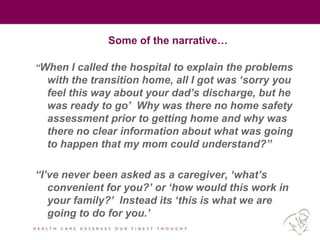
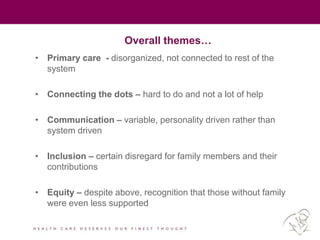
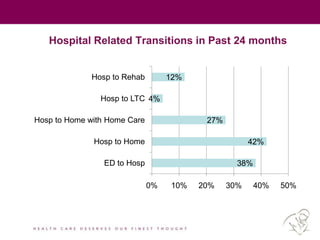
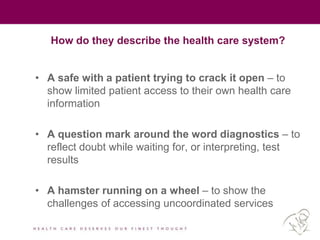
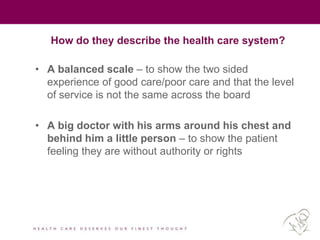
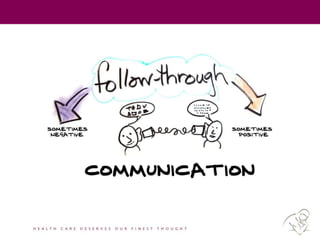
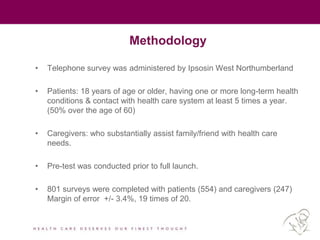
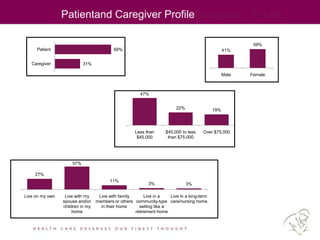
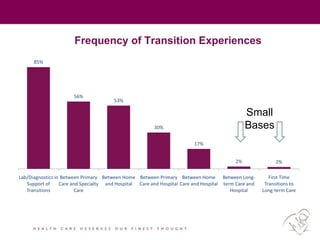
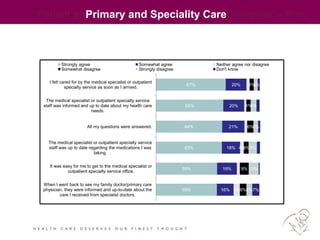
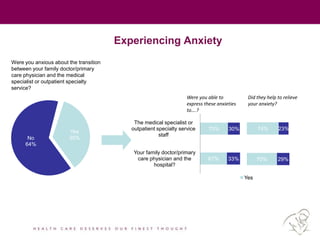
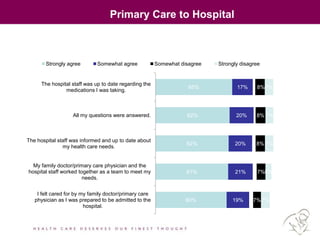
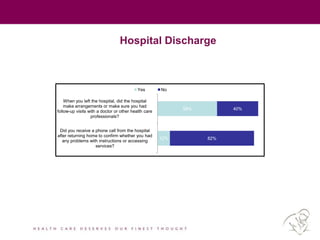
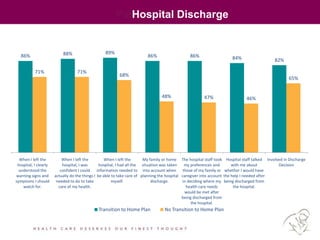
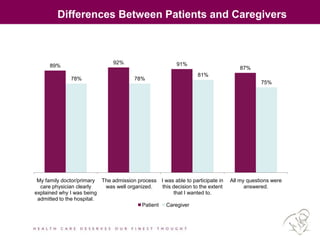
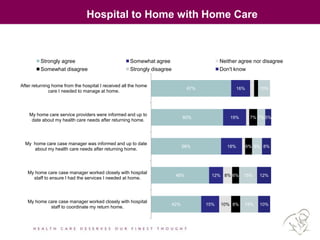
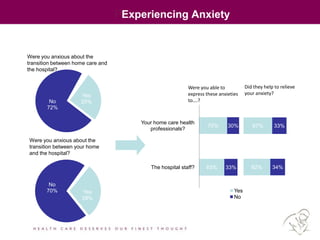
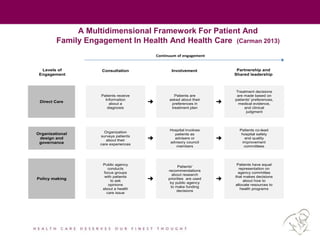
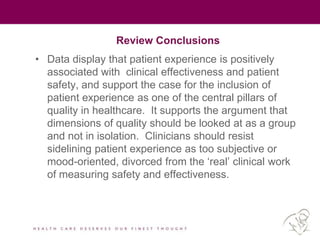
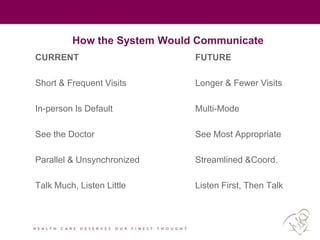
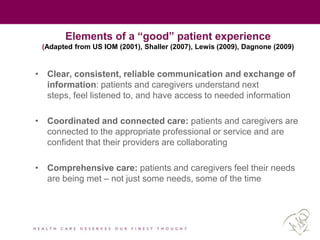
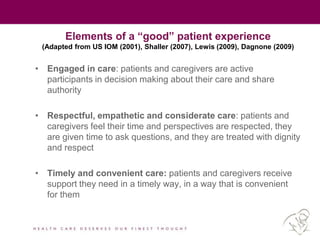
The document summarizes findings from regional consultations with seniors and caregivers about navigating Ontario's healthcare system. Key themes emerged around primary care being disorganized and unconnected; difficulty connecting services; variable communication; disregard for family members' roles; and lack of support for those without family. The document also describes a patient experience survey in Northumberland County that found transitions between care settings often lacked coordination, communication, and inclusion of patients and caregivers in decision-making. Overall, the information suggests opportunities to improve navigation, coordination, communication and inclusion across healthcare settings from the perspectives of patients and caregivers.