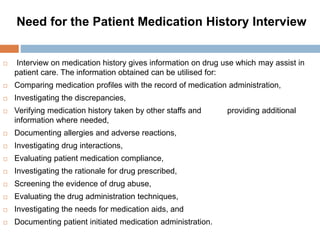
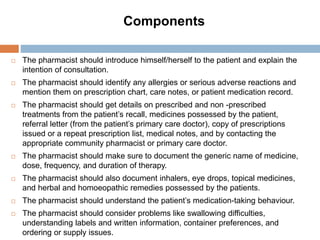
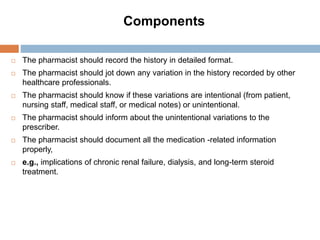
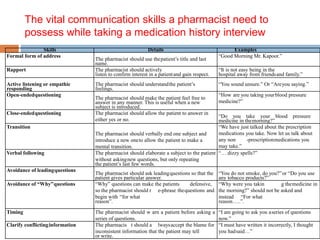
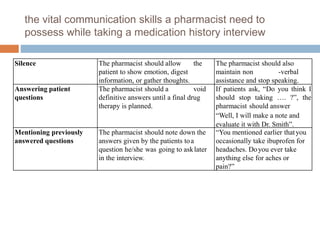
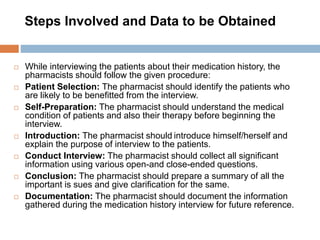
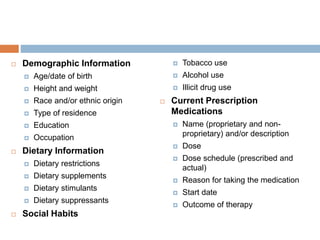
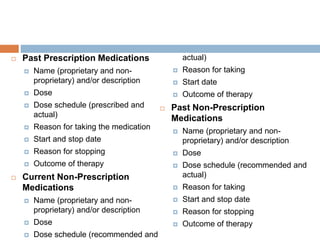
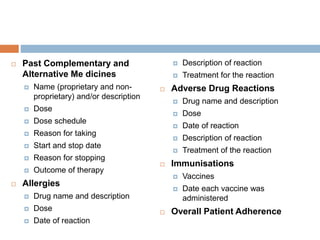
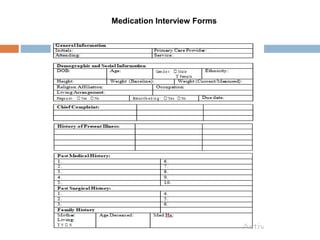
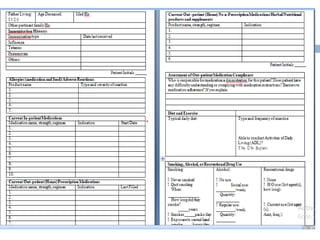
The document provides a comprehensive guide on conducting patient medication history interviews, emphasizing the importance of accurate medication histories for ensuring effective patient care. It describes the steps involved in the interview process, including obtaining essential patient information, asking relevant questions, and documenting findings. Additionally, it outlines key communication skills a pharmacist should possess to build rapport, gather information effectively, and address any inconsistencies in patient responses.