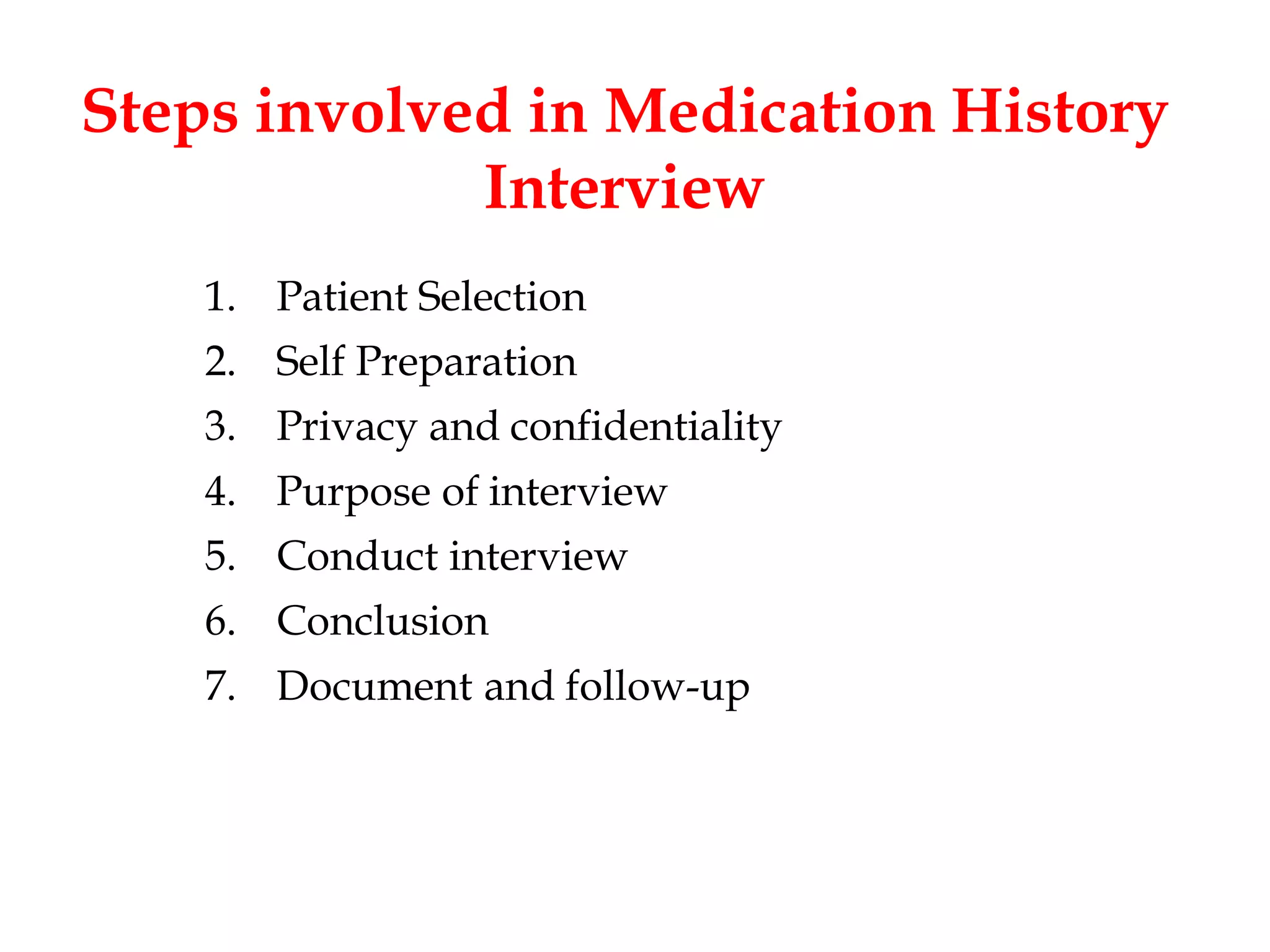
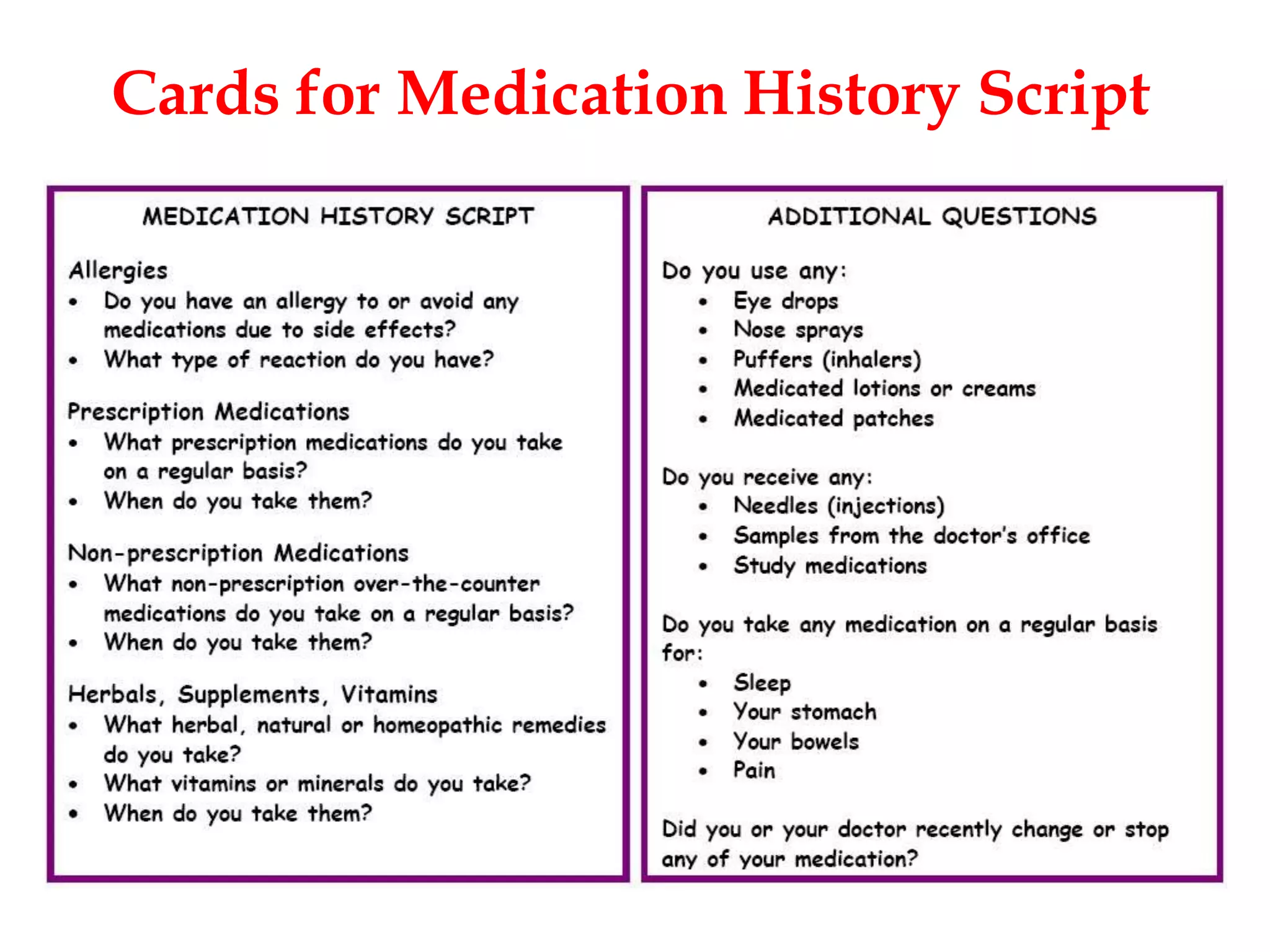
This document outlines the process and importance of taking a thorough medication history. It discusses that medication history identifies allergies and past medication use, and is the starting point for medication reconciliation and review. The goals are to obtain complete information on all prescription and nonprescription medications, perceived benefits or side effects, and allergies. This helps identify potential medication problems and develop a care plan to improve outcomes. The document then describes how to collect both subjective and objective patient data, from various sources like interviews, records, and providers. It provides a script of questions to ask patients and tips for thorough history taking. The steps of patient selection, preparation, conducting the interview privately, documenting, and following up are also outlined.