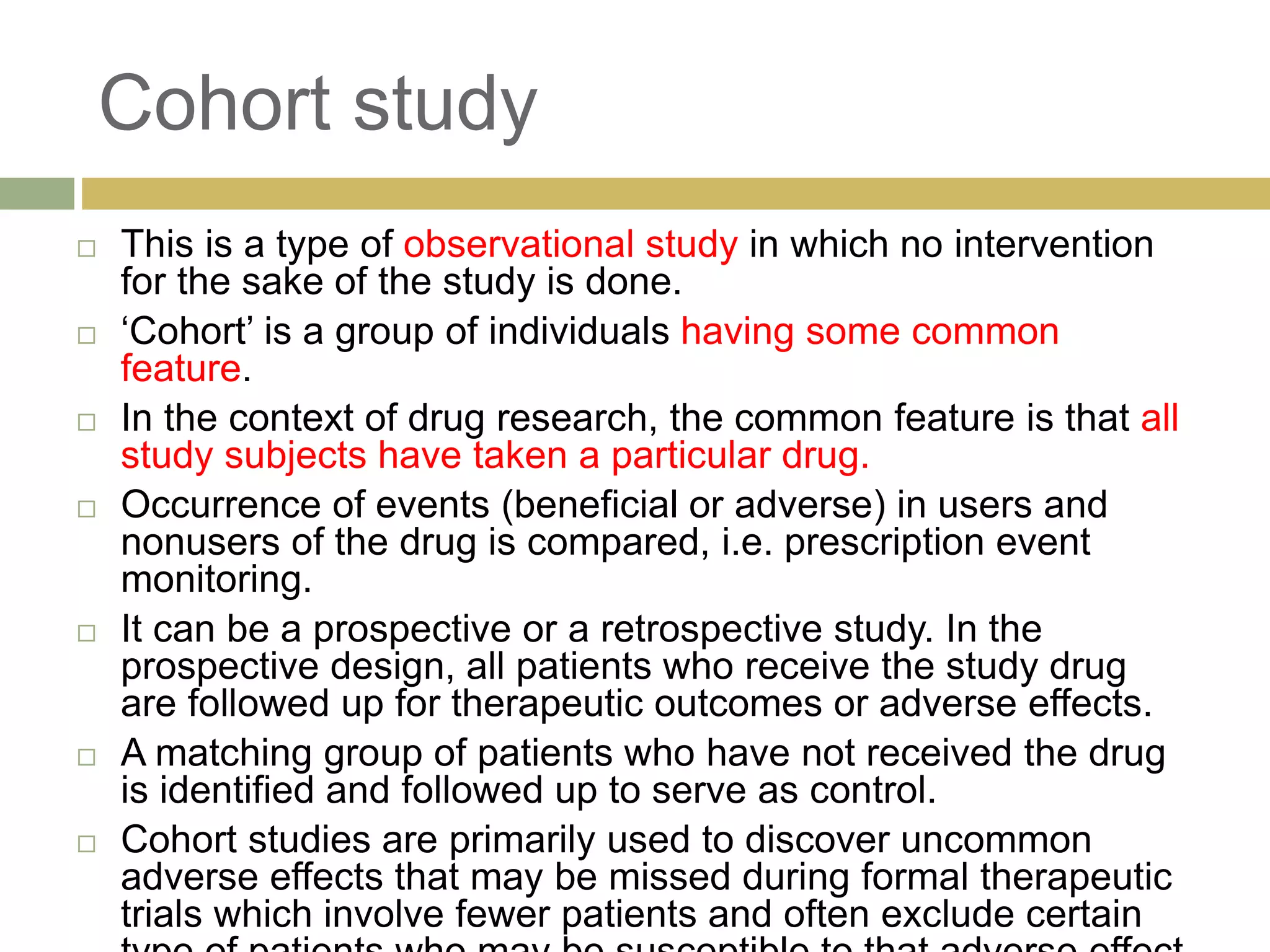
This document summarizes the different types of clinical studies, including clinical trials, cohort studies, and case control studies. It then provides detailed descriptions of clinical trials, including phases of clinical trials from pre-clinical animal studies to post-marketing surveillance. Clinical trials aim to evaluate safety and efficacy of new drugs and are conducted in a phased manner from small healthy volunteer studies to large multicenter studies in patients. Rigorous ethical and scientific standards are followed to ensure safety and quality of clinical research.