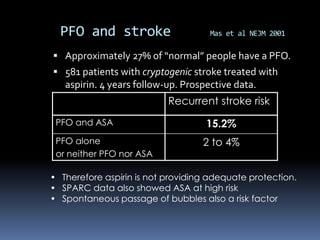
1) The CLOSURE-I trial found that percutaneous closure of a patent foramen ovale (PFO) with the STARFlex device plus medical therapy did not provide a significant benefit over medical therapy alone in preventing recurrent stroke or transient ischemic attack in patients under age 60 who had a cryptogenic stroke or TIA and a PFO.
2) The trial observed a higher rate of atrial fibrillation and major vascular complications in the device closure group compared to medical therapy alone.
3) The results were inconclusive as to whether PFO closure benefits patient subgroups based on the degree of shunting or presence of an atrial septal aneurysm.