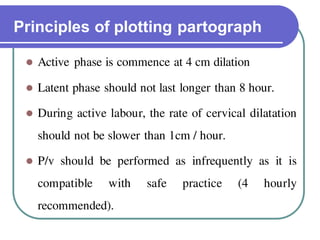
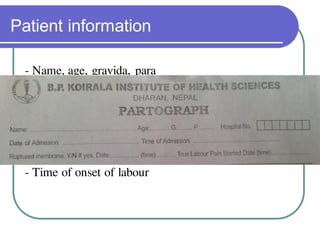
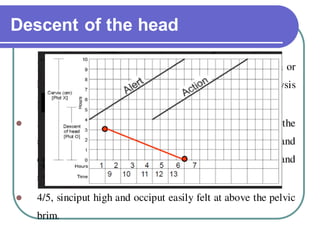
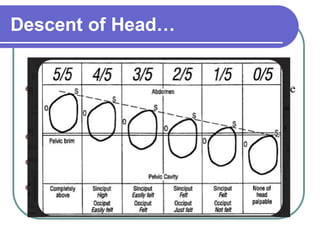
The document outlines the partograph, a crucial graphical tool used to record labor progress and monitor the conditions of the mother and fetus. It details its history, importance, advantages, components, and principles of use, emphasizing its role in early problem detection and labor management improvements. Additionally, it includes specific guidelines on plotting various factors such as cervical dilation, fetal heart rate, and maternal condition.