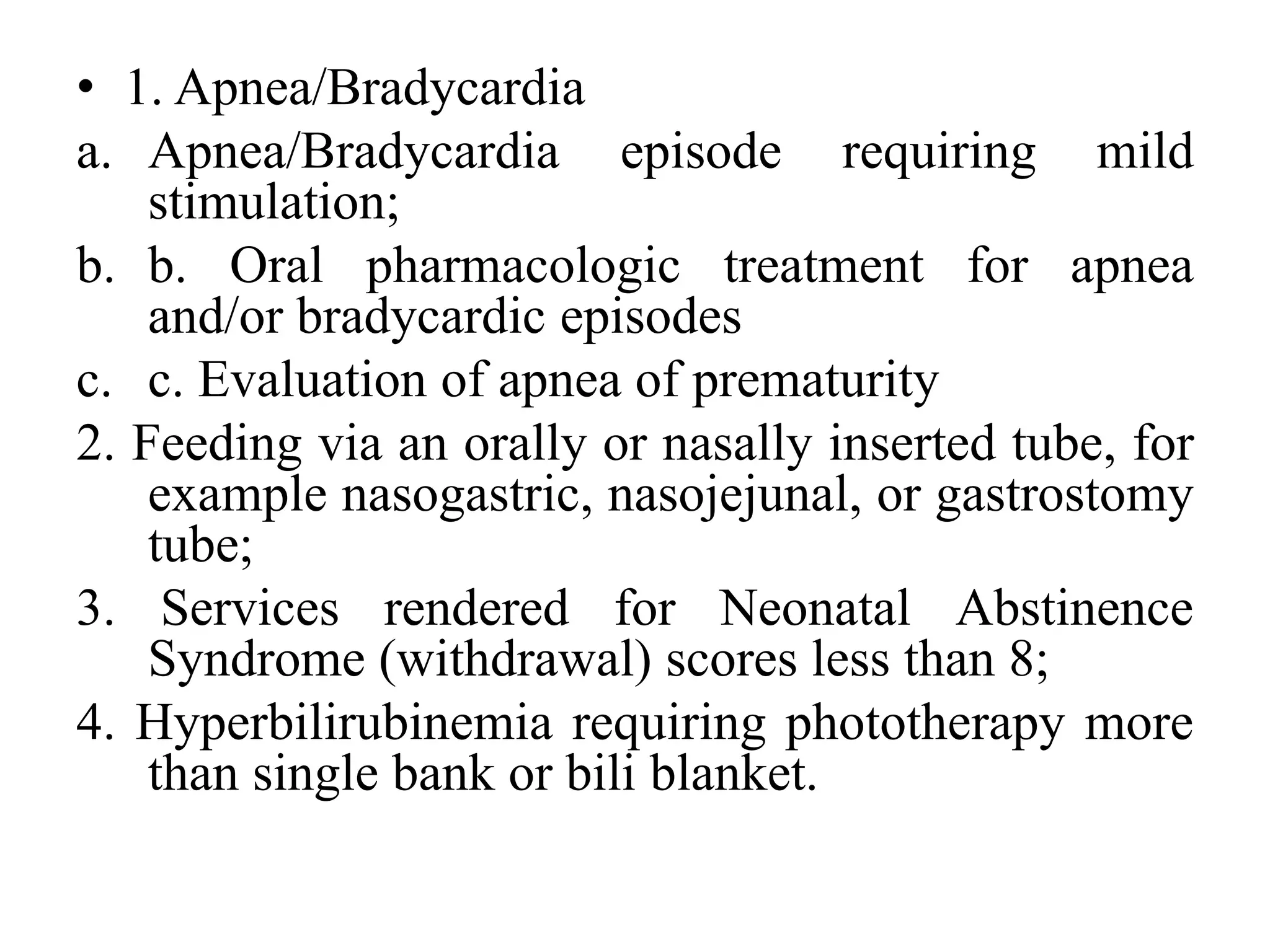
This document provides an overview of the different levels of neonatal care, from Level I to Level IV. Level I care is for stable newborns receiving routine care and observation. Level II care handles moderately ill newborns needing short-term treatment for conditions like apnea or feeding tubes. Level III is for critically ill infants requiring invasive therapies for respiratory, circulatory or metabolic instability. The highest level, Level IV, cares for very critically ill newborns needing advanced technologies and monitoring for issues such as hemodynamic instability or extracorporeal life support.




![1. Respiratory support
a. High-flow nasal cannula (HFNC) with flow less
than or equal to 3 liters per minute or
b. Supplemental oxygen via oxygen hood or low
flow nasal cannula Page 3 of 10
c. Vapotherm up to 8L/min
9. Sepsis
a. Initial sepsis evaluation (CBC, blood culture,
and other blood tests or cultures) for an
asymptomatic neonate and antibiotic treatment
pending laboratory and/or culture results;
b. b. Sepsis suspected or documented with
treatment (IV/IM [intramuscular] therapies)
beyond the initial 48 hours of treatment.](https://image.slidesharecdn.com/levelsofneonatalcare-221124094412-0e618996/75/LEVELS-OF-NEONATAL-CARE-pptx-9-2048.jpg)




![• 7. Respiratory Services
a. High-flow nasal cannula (HFNC) with flow
greater than 3 liters per minute
b. CPAP providing regulated and measured pressure
via mask, nasal or bubble devices;
c. Positive pressure ventilator assistance with
intubation and 24 hours post-ventilator care;
(Note: Intubation in the delivery room [DR]
when the endotracheal tube is removed prior to
leaving the DR or brief intubation for
administration of surfactant or deep tracheal
suctioning does not meet level III criteria for
intubation) o
d. Conditions requiring invasive intervention for
airway protection (i.e. repogle)](https://image.slidesharecdn.com/levelsofneonatalcare-221124094412-0e618996/75/LEVELS-OF-NEONATAL-CARE-pptx-14-2048.jpg)