This document discusses paediatric fractures, including physeal injuries, supracondylar fractures of the humerus, and paediatric abuse. Key points include:
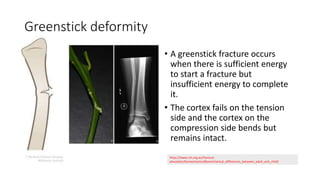
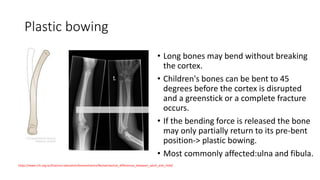
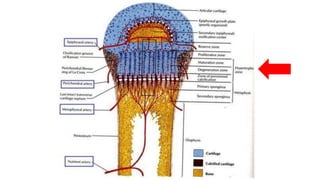
- Children's bones have a physis/growth plate not present in adults, making physeal injuries common fracture patterns like buckle fractures and greenstick fractures.
- Supracondylar fractures frequently occur in the distal humerus and can be posteriorly or anteriorly displaced. Nerve injuries and compartment syndrome are complications.
- Paediatric abuse is difficult to diagnose but risk factors include inconsistent history, delay in care, and fractures in non-mobile children. A skeletal survey aids investigation.