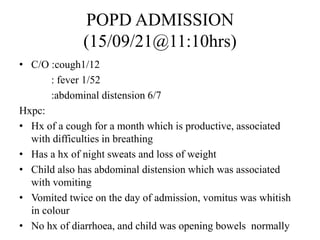
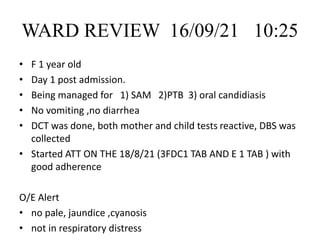
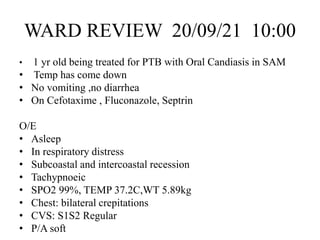
- 1 year old female child presented with cough, fever, abdominal distension, and weight loss.
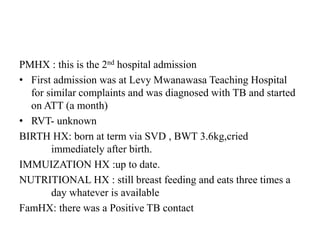
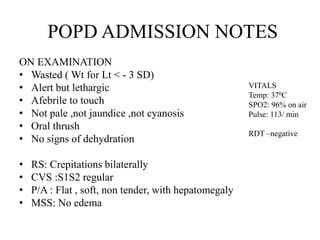
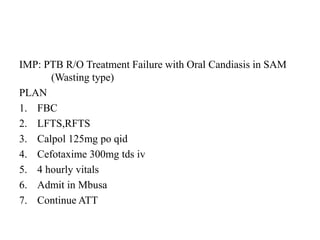
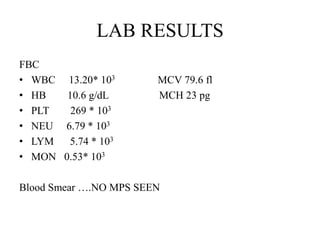
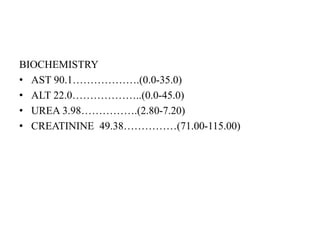
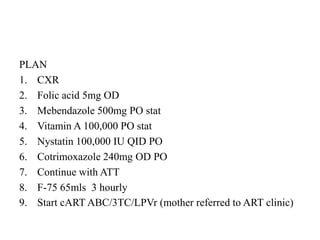
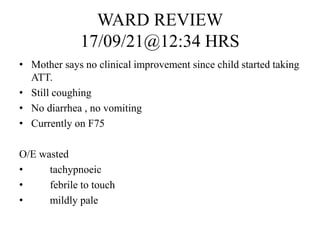
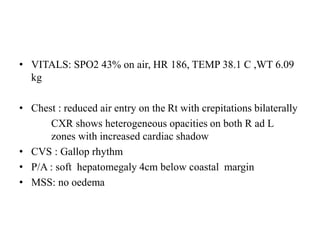
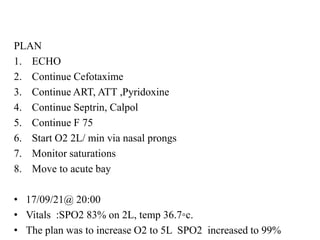
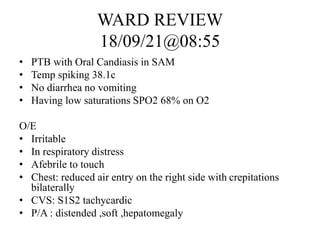
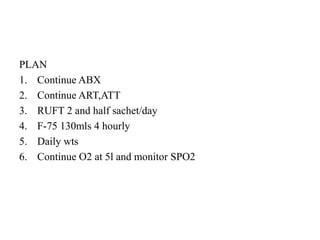
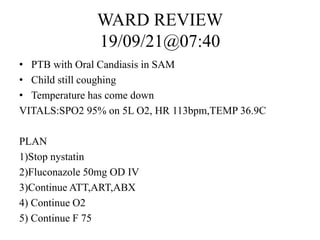
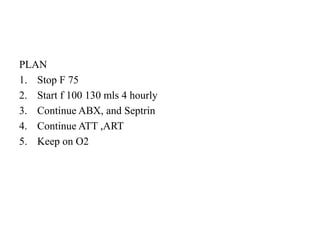
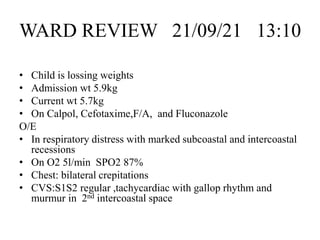
- She had been previously treated for tuberculosis but was not improving. Examinations showed respiratory distress, hepatomegaly, and low oxygen saturation.
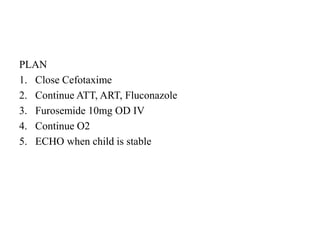
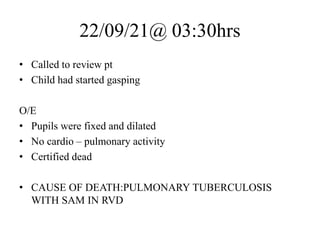
- Her condition deteriorated over her admission despite treatment. She developed respiratory failure and died. The cause of death was determined to be pulmonary tuberculosis with severe acute malnutrition.