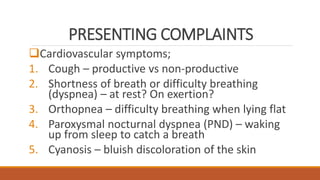
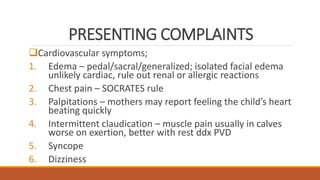
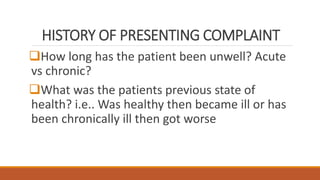
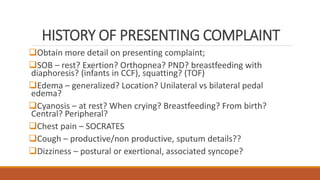
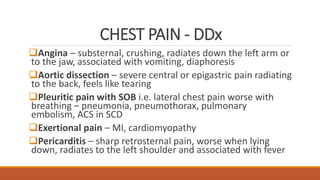
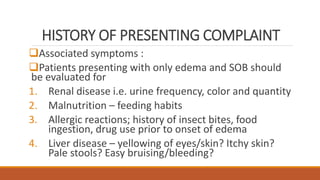
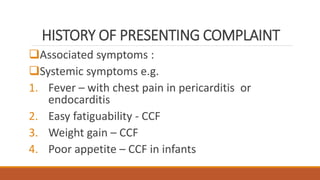
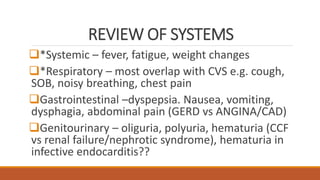
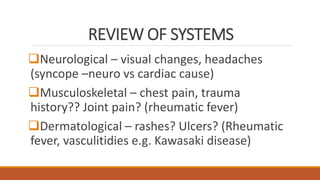
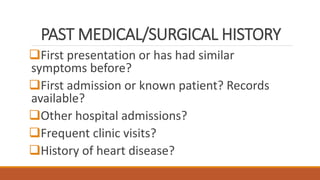
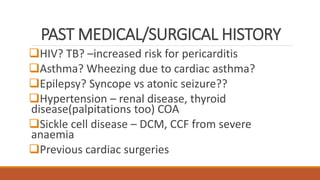
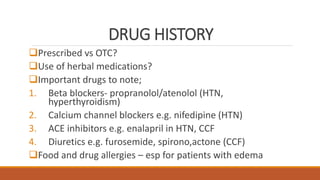
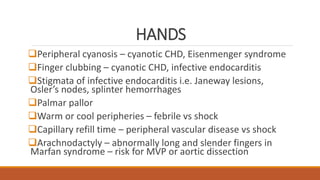
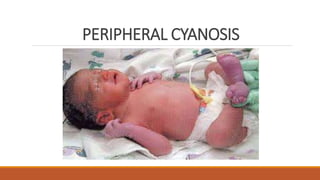
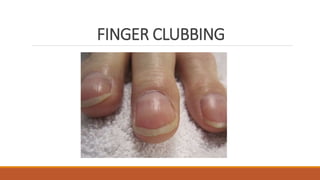
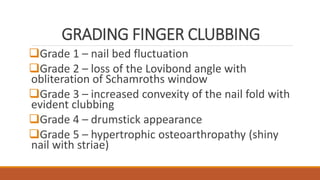
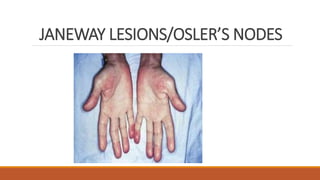
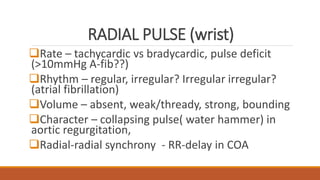
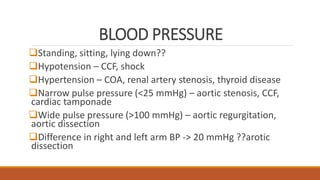
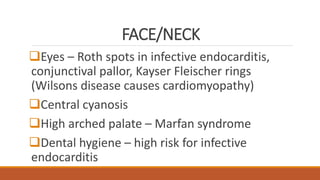
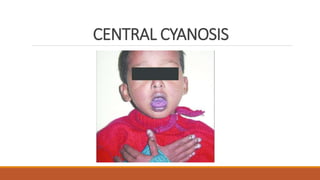
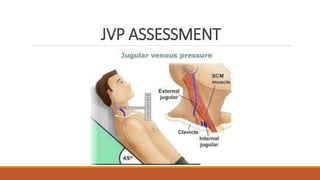
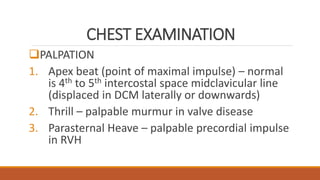
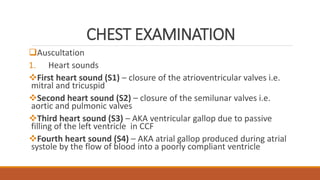
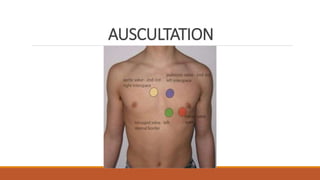
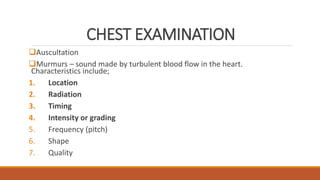
This document provides guidance on performing a cardiovascular assessment. It outlines steps to take before the assessment, including washing hands, ensuring privacy, and obtaining consent. It then describes conducting a history, physical exam, making diagnoses, and ordering investigations. The history section delves into various topics like presenting complaints, past medical history, family history, and more. The physical exam section details assessing vital signs, appearance, hands, neck, chest auscultation, and other exam maneuvers.